Varicocele: Causes, Symptoms, Differential diagnosis, Treatment
Article by Dr Raghuram Y.S. MD (Ay) and Dr Manasa, BAMS
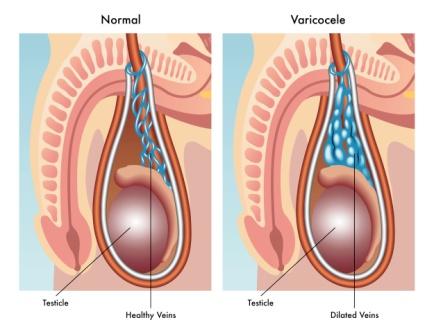
Varicocele is an abnormal enlargement or swelling of the scrotum (sac like structure which carries testes in male). This chiefly occurs due to enlargement of pampiniform venous plexus. Pampiniform plexus is a branching network of interlacing veins related to scrotum. This plexus of veins drains the testicles.
Varicocele is formed due to the dilation of testicular veins near the testis. This occurs due to defective valves in the veins or compression of the vein by a close-by structure.
Table of Contents
Causes
- Valvular incompetence of the veins draining the testis
- Pressure on the testicular veins by the surrounding structures
- Nurcracker syndrome
- Renal cell carcinoma (type of cancer)
Types
Grade 1 or Small Varicocele – The lump is small sized. It is identified only by bearing down, which increases intra-abdominal pressure, thus meddling with drainage of veins and increasing the size of varicocele. This process of identifying varicocele is called Valsalva maneuver
Grade 2 or Medium or Moderate Varicocele – The lump is medium sized. It is identified by palpation without bearing down (Valsalva maneuver)
Grade 3 or Large Varicocele – The lump is the largest in size. It is easily identified by visual inspection alone.
Epidemiology
Epidemiology (U.S. National Library of Medicine) –
- Varicocele occurs in about 20% of all men
- It is diagnosed in 15,000 of 100,000 adult men
- It is diagnosed in 40,000 of 1000,000 men with reduced fertility
- It increases with age until adulthood
- Incidences vary with age, the rate is higher at adolescence and into adulthood
Occurrence rate:
- 800 of 100,000 boys aged between 2 to 6 years
- 1000 of 100,000 boys aged 7 to 10 years
- 7,800 of 100,000 boys aged 11 – 14 years
- 15,000 of 100,000 boys aged older than 15
Signs and Symptoms
- Swelling – Swelling in the scrotum or lump in the testicles is either seen or felt
- Enlargement – Enlarged veins of the scrotum (around testis) which are visible or can be felt with fingers (palpable swelling of veins)
- Pain – Pain in the scrotum and testis which is dragging-like or aching in character, it may be sharp or dull in character
- Heaviness – Feeling of heaviness in testicle or testicles
- Atrophy – Shrinking of the testicle / testicles
- Alteration – of testesterone (hormone) levels
- BPH – Benign Prostatic Hyperplasia (enlargement of prostate gland, a gland located at the bottom of urinary bladder in men)
- Urinary problems – as a consequence of BPH
Causes and pathogenesis
There are lots of veins (network) around the spermatic cord. When the valves within these veins do not function properly, varicocele occurs. This failure of valves results in backflow of blood into the pampiniform plexus in the scrotum. (Valves of the veins should function properly to push the blood against gravity in an upward direction. If the valves fail to function, the blood instead of moving upwards flows back and downwards leading to stagnation. This leads to swelling, fluid collection and other complications. When this mechanism happens in the veins around the scrotum, varicocele occurs).
The venour backflow increases the diameter of the vein because of excessive pressure and testosterone pooling.
The pooled blood is toxic and may cause damage to the veins and also the testicles.
Varicocele is a gradual process, develops slowly over a period of time and in many instances may not have any symptoms.
Varicocele is most frequently diagnosed in the age group of 13-30 years. They occur in about 20% of all males.
Points of Interest
Most idiopathic varicoceles occur on the left side since the left testicular vein travels superiorly and connects to the left renal vein (at 90 degree angle). On the other hand, the right testicular vein drains directly into the inferior vena cava. Isolated right sided varicoceles are rare to find.
Secondary varicocele – This occurs due to the compression of the venous drainage of the testicle. Pelvic or abdominal malignancy are also contributory. Nutcracker syndrome is a non-malignant cause of secondary hydrocele. In this, the superior mesentric artery compresses the left renal vein, causing high pressure there to be transmitted into left pampiniform plexus. The most common cause is renal cell carcinoma (hypernephroma) followed by retro-peritoneal fibrosis or adhesions.
Lifestyle
Below mentioned factors can affect both the rate of occurrence and severity of varicocele symptoms:
- Type of activity
- Diet
- Bowel health
- Testicular temperature
- Smoking
- Alcohol etc
Pathophysiology
The pampiniform plexus (venous network that drains the testicle) travels along the back of the testicle, along with epididymis and vas deferens, and then into the spermatic cord. This network coalesces into the gonadal or testicular vein. The right gonadal vein drains into the inferior venacava. The left gonadal vein drains into the left renal vein at right angle to the latter. The renal vein later drains into the inferior vena cava. One of the chief functions of the plexus is to lower the temperature of the testicles. Varicocele causes loss of this function. Therefore the most common complication of untreated varicocele is higher temperature of the testes. This later results in testicular atrophy leading to infertility.
Pathophysiology
Pampiniform plexus of veins are made up of small vessels. Their measurement ranges normally ranges from o.5 to 1.5 mm in diameter. Dilation of these vessels more than 2 mm is called varicocele.
The harmful effect of varicocele on the sperm production is progressive. Due to the reduction in supply of oxygenated blood and nutrients to the sites of sperm production due to the impact of varicocele, persistently reduces the quality and quantity of the sperms. This leads to the reduction in the fertility capacity of sperms with time.
Varicocele and BPH – As an effect of varicocele, the blood from the testes cannot drain via pampiniform plexus. This blood changes its course and routes through the prostate gland in a process called communicating vessels. This increased blood flow to the prostate can lead to congestion and enlargement of the prostate gland. This is called as BPH or Benign Prostate Hypertrophy. This occurs through physical mechanisms and also due to accelerated prostate cell growth (proliferation) resulting from extremely high concentration of free testosterone reaching directly from the testes to the prostate.
Diagnosis
Palpation – On palpation of scrotum, one can feel a non-tender (not painful on touch), twisted mass along the spermatic cord. It is compared to ‘feeling a bag of worms’.
On seeing – the testicle on the side of the varicocele may or may not be smaller than the other side.
Ultrasound (USG) – It is a reliable way of diagnosing varicocele. Ultrasound will show the dilation of the vessels of the pampiniform plexus to greater than 2 mm in measurement. The patient should undergo a provocative maneuver like ‘Valsalva’s maneuver’ (attempting expiration against a closed airway) or standing up during the exam. Both these maneuvers are designed to increase the intra-abdominal venous pressure and increase the dilation of the veins.
Doppler ultrasound – It is a technique of measuring the speed at which the blood is flowing in the vessel. An ultrasound with a doppler mode helps to see blood reverse the direction in a varicocele with a Valsalva, thus increasing the sensitivity of the examination.
Treatment
Surgery
There is tentative evidence that surgery of varicocele may improve fertility. Inguinal (groin using percutaneous embolization), retro-peritoneal (abdominal using laparoscopic surgery) and Infra-inguinal / sub-inguinal (below the groin) are the 3 most common approaches of surgery in varicocele.
Ice packs – should be kept to the afflicted area for the first 2 days after surgery, to reduce swelling. The patient should be advised to wear a scrotal support for some time after surgery.
Surgical Repair –
Surgical repair of varicocele is the most effective and the most cost-effective treatment (in the long run). Varicocele repair has shown to improve semen analysis, thus improving fertility. It also improves pain and discomfort dramatically. Further damage of the testes can be stopped with surgical intervention. All surgical methods involve ligation of affected veins to prevent abnormal blood flow. Varicoceles are seen to re-appear after surgery, but the recurrence rate is low, usually less than 10%.
Surgical repair is recommended for men with the below mentioned signs and symptoms –
- Severe pain or discomfort in the testes
- Testicular atrophy – surgery should be done if the atrophy (volume and length of testes is below a certain threshold) has already taken place
- Infertility (in presence of infertility and to prevent further damage to the testes)
- Grade 2 or 3 varicoceles (those having moderate or large varicocele and an abnormal semen count)
- Bilateral varicoceles
Methods of surgical approach –
Varicocelectomy via open incision – is a surgical procedure for correction of a varicocele. Different surgical techniques are followed. The varicocele is reached from an incision just above or below the scrotum.
Varicocelectomy via laparoscopy – In this, using the laparoscopic technique, the surgeon makes 3 tiny incisions in the patient’s abdomen and passes small surgical instruments through the incisions and to repair the varicocele.
Varicocele embolization – Embolization of affected veins is an alternative to a varicocelectomy. It involves a small wire being passed through a peripheral vein and with the use of a catheter; the surgeon obstructs the vein in the abdomen which is transmitting increased pressure to the testicle.
Normal activity may be resumed 2 days after surgical repair of a varicocele. Exercise should only be resumed 2-4 weeks post-surgery.
Semen samples for analyses are obtained 3-4 months after the correction procedure and then repeated again after 6 months. Improvement in sperm count is noted often within 6 months after surgery, but may not be observed until 1 year after the procedure.
Non surgical management
Non-Surgical Management of Varicoceles
There is actually no effective medical treatment of varicoceles. Medical management is focused on symptomatic relief of discomfort and pain.
Non-steroidal anti-inflammatory drugs – These mainly help in pain relief. It is not disease specific but is symptomatic approach. Surgery should be considered if pain continues in spite of using NSAIDs.
Supportive underwear – can help to relieve some pain as it assists with blood flow. Underwear should be supportive and not restrictive.
Lying down – relieves some pain caused by a varicocele. The relief is slight and temporary.
Surgery complications
Possible complications of surgery:
- Haematoma (bleeding into tissues)
- Hydrocele (accumulation of fluid around the affected testicle)
- Infection
- Injury to the scrotal tissue or structures
- Injury to the artery that supplies the testicle
Embolization
Embolization is an alternate to surgery in varicocele. It is a minimally invasive treatment for varicocele. It is performed by an interventional radiologist. In this, a small wire is passed through a peripheral vein and into the abdominal veins that drain the testes. The doctor can obstruct the gonadal vein through a small flexible catheter so that the increased pressures from the abdomen are no longer transmitted to the testicles. The obstruction is often performed with small metal coils, many in number. The testicles then drain through small collateral veins.
Advantage – the recovery in this procedure is significantly less than with surgery. The risk of complications is also minimized with overall effectiveness similar to the surgery. Recurrence rates are less. But there is a risk of testis being exposed to the radiation in this procedure.
Points of interest
Microsurgical testicular sperm extraction (Micro TESE) and deferring varicocele repair – might help the couples who are infertile, secondary to non-obstructive azoospermia and concurrent varicocele
Varicocele can reduce testosterone production in both testes due to increased temperature from the great volume of backed up blood in the varicocele veins. Leydig cells ability to produce testosterone is reduced in those suffering from varicocele.
According to some studies, the blood testosterone levels have increased in individuals who have undergone varicocele repair.
Prognosis
Varicocele can be harmless. In some cases it can cause pain and infertility. Though some studies show that there is improvement in sperm quality following surgery, the other studies show that the regular surgery has no significant effect on infertility. Thus the surgery may not improve fertility. The patient might have to undergo a non-surgical treatment.
Study
A 2012 Cochrane review – found tentative but unclear evidence of improved fertility among males treated for varicocele. The benefit may be as large as one per seven men treated.
Click to Consult Dr Raghuram Y.S. MD (Ayu)








3 comments
benedict
I want to know the treatment, is it necessary to get surgery for prevention of prostrate issues
Jit
Hi Doctor, Is the treatment for BPH (Enlarged Prostate) the same as for varicocele?
Thanks.
Dr J V Hebbar MD(Ayu)Author
No.