OsteoArthritis Symptoms, Prevention, Lifestyle tips, Ayurvedic treatment
Article by Dr Raghuram Y.S. MD (Ay)
The ends of 2 or more bones come together to form joints of our body. There are many bones in our body which hold on to their counterparts to form various joints. The joints connect various parts of our body and enable free movements. We are assembled and integrated as one piece because of the joints which hold on to the bony ends participating in that joint.
All our day to day activities like sitting, standing, jumping, running, walking, bending, stretching, holding etc depends on the integrity and healthy condition of our joints. We cannot imagine living and leading our life easily with painful, swollen and stiff joints. There are many diseases or disorders which afflict our joints at some part of our life. Many give pain and distress, others disturb our living.
Osteoarthritis is one such disease which when afflicts our joints makes us feel that life is definitely a curse!
Osteoarthritis – Osteo meaning bones and Arthritis meaning painful inflammation and stiffness of the joints.
Osteoarthritis is called as Sandhigata Vata in Ayurveda. Sandhigata Vata means the invasion and localisation of morbid Vata or Vayu in the joints of the body thereby producing pain, swelling and disturbed movements.
Table of Contents
Etymology
OA is derived from the Greek word part osteo- meaning ‘of the bone’ combined with arthritis, arthr- meaning ‘joint’ and itis- meaning ‘inflammation’. The –itis of OA is misleading as inflammation is not a conspicuous feature of OA. Some clinicians refer to this condition as osteoarthrosis to signify the lack of inflammatory response.
What is Osteoarthritis?
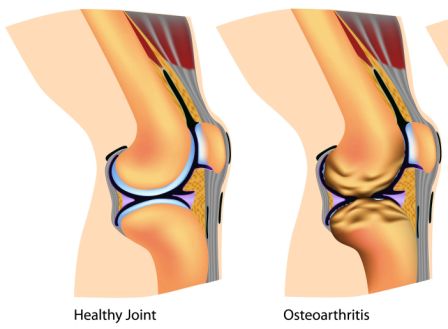
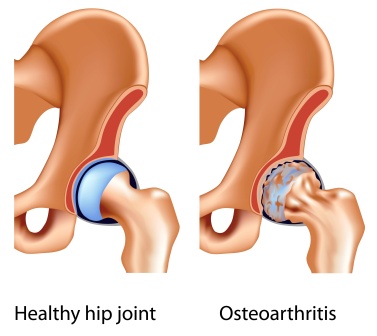
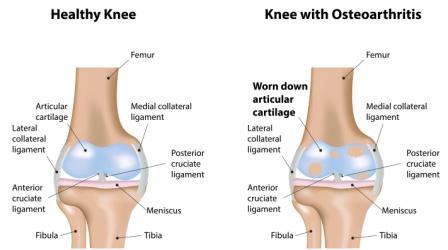
Osteoarthritis is the common form of arthritis. It afflicts millions of people throughout the world. Osteoarthritis occurs when the protective cartilage on the ends of your bones wears down over a period of time i.e. it results from the breakdown of joint cartilage and underlying bone. OA can affect and damage any joint in the body.
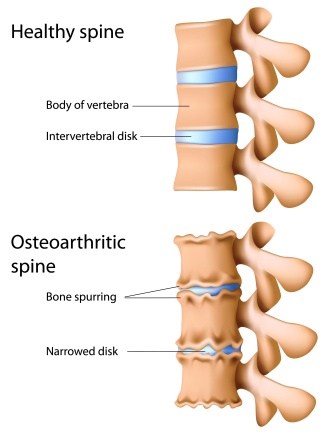
Joints of the hands, Joints near the finger ends, base of the thumb, neck, lower back, hips, knees and spine are commonly afflicted by osteoarthritis. Joints on one side of the body are often more affected than those on the other. Unlike other types of arthritis, only joints are typically involved in OA.
The most common symptoms are joint pain and stiffness. Joint swelling and decreased range of movements are also present in many cases.
It gradually worsens with time and no cure exists. Active life, maintaining healthy weights, effective medicines and treatments may slow the progression of osteoarthritis and thus may help to improve pain and joint function.
Other names – Degenerative arthritis, Osteoarthrosis, Degenerative Joint Disease (DJD)

Diet for Arthritis
By Sharmishta Majumdar – [email protected]
Breakfast: 7-7:30 AM
Midday Snack: 10:30 AM
Lunch: 12:30 – 1 PM
Evening Snack (only if stomach-wrecking hunger strikes): 4:30 Pm
Dinner: 6:30 -7 Pm
Best Grains: Wheat, Oats, Rice, Millets (in small quantity)
Best Legumes (Unpolished): Black Gram (Urad), Moong
Best Vegetables: Sweet Potato, Onions, Garlic, Raw Papaya, Sweet Peas, Ginger, White
Potatoes (best taken as curry with warming spices), Squash, Yams, Cauliflower, Beets, Carrots,
Beans (not in excess), Cilantro (Coriander Leaf), Tomatoes, Bottle Gourd, Ash gourd, Okra
Nuts (Soaked for overnight)/ Seeds: Almonds, Cashews, Lotus Seeds (served with sugar and
ghee), Pecan, Pinon, Pistachio, Sesame Seeds (in form of chutney), Walnut
Dairy: Non-pasteurized Cow’s Milk (boiled with warming spices like cinnamon, cardamom and
bay leaf), Fresh Butter, Soft Cheese (Paneer), Cream (use fresh in small quantity; heavier so hard
to digest), Ghee, Takra (served with roasted mild spice powder of coriander, fennel, cumin,
cardamom and a little bit of dry ginger), Ghee
Best Animal Products: Duck Meat (cook with carminative spices; harder to digest than turkey
or chicken), Chicken (cook till tender in gravy), Fish (both ocean & fresh water varieties), Eggs
(Preferably organic, in curry form), Goat’s Meat/Mutton
Best Fruits (Fresh & Seasonal): Cooked Apples (served with cinnamon powder), Apricots,
Plums, Banana, Grapes, Cherries, Soaked Dates, Coconut, Figs (Anjira), Pears (baked with
warming spices), Grapefruit (small quantity), Lime, Mango, Oranges, Papaya, Pineapple,
Strawberries, Avocado
Best Oils (Only cold-pressed options for cooking): Coconut, Mustard, Sunflower, Olive,
Sesame (good for sautéing not deep frying)
Best Sweeteners: Jaggery
Best Spices (use in moderation): Ginger, Cloves, Black Cumin (Kalonji), Mustard, Wild
Celery, Nutmeg, Cumin, Coriander, Cardamom, Saffron, Bay Leaf, Black Pepper, Long Pepper,
White Pepper, Cinnamon, Clove, Asafetida, Turmeric, Black Salt, Himalayan Rock Salt
Restrictive Foods: Raw Salads; Spicy Foods (Pungent taste), Refrigerated/ Stale Foods,
Refined Sugar; Ice Cream; Yogurt, Fried Sweets; Mushrooms, Deep Fried Snacks; Leafy
Greens, Tandoor/ Roasted Meat, Fish or Vegetables; Packaged Fruit Juices; Aerated Drinks;
Coffee/ Team; Dark Chocolates
Breakfast Recipes:
- Oats Upma
- Rava Upma
- Soft Paneer Paratha served with fresh butter and tangy mint coriander chutney
- Carrot Beetroot Paratha with small quantity of homemade lime or sweet mango pickle
- Mixed Grain Idli / Dosa/ Uttapam Served With Sambar And Coconut Chutney (made
with oats + rice + rava + urad daal flour) - Light Vegetable Dalia
- Sabudana Kichidi
- Creamy Millet/ Oats Porridge (cook this recipe with overnight pre-soaked millets, milk &
½ tsp. cinnamon powder)
Rava Halwa (prepared with jaggery and ghee)
Substitute Tea / Coffee with Ginger – CCF Tea
How to prepare: Boil 1 glass of water with ¼ tsp. of crushed fresh ginger + 1 tsp. of cumin seeds - 1 tsp. coriander seeds and 1 tsp. fennel seeds. When the liquid reduces to 1 cup, add little
jaggery powder and enjoy!
Mid-day Snack: A whole fruit or Soaked 4-5 pieces of nuts or One Cup of Takra
Lunch Recipes:
- Aged Rice/ Chapattis served with 1tsp of Ghee / Mix Vegetable Pulao (once a week)
- Sambar Dal (cooked with different assortments of vegetables) / Light Daal Tempered
with ginger, turmeric and cumin seeds - If vegetarian: Few popular options are Paneer Aloo Matar Curry/ Butter Paneer/
Paneer Bhurji/ Kadai Paneer - If non- vegetarian: Chicken Soup / Egg Curry / Fish Curry/ Mutton Curry
- One boiled vegetable stew (with / without thin coconut milk) / Cauliflower Curry/
Carrot Beans Beetroot Peas Stirfry (not too dry)/ Raw Papaya Soya granules Curry
Desserts (once a week preferably made in ghee with gur): Carrot Halwa / Rasgullas/
Coconut Barfi / Tomato Date Chutney/ Rasmalai / Oats Halwa/ Atta ka Sheera/ Sabudana
Kheer/ Payasam
Snacks:
- Half glass of non-pasteurized cow’s milk (preferably A2 variety) boiled with
cardamom, bay leaf and served with a pinch of turmeric - Upma
- Uttapam
- Boiled Sweet Peas/ Carrots sprinkled with roasted cumin powder, crushed black
pepper and black salt
Dinner:
- Chapati/ Basmati Rice + Boiled Veg Curry
- Runny Khichdi
If suffering from constipation ½ cup warm milk with 1 tsp. ghee 2 hours before going to bed.
Prevention tips
Lifestyle tips, Prevention of Osteoarthritis –
Osteoarthritis is caused by wear and tear on the cartilage that protects and cushions your joints. Some risk factors for OA are inevitable, such as:
Heredity
Gender
Age
Therefore, OA will never be entirely preventable. However, other risk factors can be modified. We can do a lot of things which can reduce the risk of OA. Anyhow, if OA develops, many of the same lifestyle changes can also slow down the course of the disease.
Most of us will have X-ray evidence of OA as we suffer from various degrees of stiffness and pain in the joint. OA can be prevented by following the below said measures. The same measures help in halting the progression of OA. Thus lifestyle changes and prevention go hand-in-hand in OA.
The below mentioned Lifestyle changes will help in preventing OA and also helps in healing pains and related complaints if the disease has started to manifest
Exercise – It can increase endurance and strengthen the muscles around your joint. It makes your joints stable. Walking, biking and swimming are the best in business. Overdoing exercises can also give you new pain. It indicates that you need to take a break and continue it later. Quality and quantity of exercise shall be determined before starting.
Exercises can slow down or prevent OA. They –
- Help maintain healthy joints
- Relieve stiffness of joints
- Reduces pain and fatigue
- Increases muscle strength
- Increase bone strength
Look for activities and exercises that are not just aerobic. They should also include strength training and stretching
Exercises
Exercises for Osteo arthritis:
Quadriceps strengthening exercises: Todd P.Stitik, MD, professor of physical medicine and rehabilitation at UMDNJ-New Jersey Medical School recommends isometric moves and wall slides to improve the strength of Quadriceps muscles (muscles at the front of your thighs).
To do these – stand with your back to a wall, with feet kept shoulder width apart. Now lean back against the wall, placing your feet out in front of you as far as you comfortably can. Bend at the knees, put your hands on your waist, and slide with your spine, maintaining contact with the wall until you reach a sitting position. Your knees should not bend more than 90 degrees. Then slowly slide back to your original position. Repeat 8-10 times.
4 good exercises for OA –
The below mentioned exercises will help you in OA
Standing calf stretch
Seated hip march
Quadriceps stretch
Hamstring stretch
Related exercises
Other exercises for OA – Read here
More useful exercises for OA – Read here
Videos for beneficial exercises in OA –
Knee OA –
Shoulder OA –
Hip OA –
Hip OA –
Rest –
Exercises can help develop healthy joints and muscles. But overuse of joints can increase the risk of developing OA. Important thing is maintaining balance between these two. Rest to the joints is equally important as is the exercise. If you have painful or swollen joints, give them a break. Try to avoid using a swollen joint for at least ½ – full day. Letting an injured joint heal may reduce the risk of developing OA in future. Fatigue has shown to increase pain in those having OA. Make sure you get enough sleep every night.
Good postures – alleviates stress on many joints. So it is important to maintain the 2 natural curves of your spine whether sitting or standing.
Avoid repetitive movements –
Doing the same movements or motions again and again during work or sports puts you at increased risk of developing OA. Ballet dancers, professional athletes and construction workers are at risk. This can also occur with activities like golf and tennis. Make sure that you avoid the repetitive motions as far as possible. Change your routines regularly; vary your movements as much as you can.
Avoid injuries or get them treated: Suffering a joint injury when you are young, predisposes you to OA in the same joint when you are older. Injuries caused when you are an adult are greater risk.
To avoid joint injuries when exercising or playing sports, the National Institute of Arthritis and Musculoskeletal and Skin Diseases recommends the following:
- Avoid bending knees past 90 degrees when doing half knee bends
- Keep feet as flat as possible during stretches to avoid twisting knees
- When jumping, land with knees bent
- Do warm-up exercises before sports, even less vigorous ones such as golf
- Cool down after vigorous sports
- Wear properly fitting shoes that provide shock absorption and stability
- Exercise on the softest surface available, avoid running on asphalt and concrete
- Get prompt treatment if you already have a joint injury. Later take steps to avoid further damage, such as modifying high-impact movements or using brace to stabilize the joint
Managing occupational risk –
- Jobs that involve a lot of repetitive motion can harm your joints. Talk to your doctor about ways to reduce your OA if your job involves a lot of:
- Kneeling
- Lifting
- Twisting
- Walking
- You should work and alter the way you perform these activities
Weight loss – being obese or overweight can increase the stress on your weight bearing joints such as knees and hips. Even a small amount of weight loss can relieve some pressure and reduce your pain. Weight reduction should be done after appropriate planning in consultation to your health care provider or doctor. Changes in diet and skillful inclusion of various forms of exercises can do wonders in relieving symptoms of OA.
Control Blood Sugar: Latest research suggests that Diabetes Mellitus which affects the body’s ability to regulate blood sugar (glucose) may be a significant risk factor for OA. That’s because high glucose levels speed the formation of certain molecules that make cartilage stiffer and more sensitive to mechanical stress. Diabetes can also trigger systemic inflammation that leads to cartilage loss.
Heat and cold application
Applying over-the –counter pain creams and gels
Use assisting devices – They help relieving stress on your painful joints and help to lead day long activities easily. Example, holding a cane while walking.
Right eating habits – No specific diet has been shown to prevent OA. Certain nutrients have been associated with a reduced risk of the disease or its severity. They are:
Omega-3 fatty acids – They are healthy fats, shown to reduce joint inflammation. Good sources of Omega3 fatty acids are – fish oil, certain plant / nut oils including walnut, canola, soybeen, flaxseed / linseed and olive
Vitamin C – reduces the risk of OA progression. Sources include green peppers, citrus fruits and juices, strawberries, tomatoes, broccoli, turnip greens and other leafy greens, sweet and white potatoes and cantaloupe.
Vitamin D – Low vitamin D is related to OA progression. Sources include exposure to sunlight, fatty fish such as salmon, mackerel, tuna, sardines, and herring, vitamin D fortified milk and cereals and eggs.
Include Ginger – Ginger is a wonder remedy in many aliments. It reduces muscle pain and joint inflammation. Ginger can be used in the form of food inclusion, tea, supplement or hot ginger compression on sore joints.
Eat onions and garlic – Diallyl sulphides, the compounds known as alliums found in garlic, onions and leeks inhibited the enzymes that cause joints to degenerate (2010 study of King’s college London)
Enjoy Non-citrus fruits – Fruits such as berries, apples, plums and peaches contain antioxidants that may decrease inflammation. Those who eat these types of fruits frequently were found to have less development of OA than those who didn’t. Related
Yoga for OA
Yoga for OA –
Virabhadrasana (Warrior pose) –
Baddha Konasana (Butterfly pose) –
Dandasana (Staff pose) –
Padangushtasana (Big Toe Pose) –
Setu bandha sarvangasana (Bridge pose) –
Adho Mukha Svanasana (Downward facing dog pose) –
Ardha chandrasana (Half moon pose) –
Uttanasana (Forward bending pose) –
Utthita Hasta Padangushtasana (Extended hand to big toe pose) –
Utthita Parshvakonasana (Extended Side Angle Pose) –
Hatha Yoga –
Most forms of Yoga in the west can be classified as Hatha Yoga. Hatha refers to the practice of physical yoga postures, meaning your Ashtanga, Vinyasa, Iyengar and Power Yoga classes are all Hatha Yoga. The word Hatha can be translated as ‘willful’ of ‘forceful’ or the yoga of activity, and as ‘sun’ (ha) and ‘moon’ (tha), the yoga of balance. Hatha practices are designed to align and calm your body, mind and spirit in preparation for meditation.
Hatha Yoga is said to be highly effective in OA. Read more
Home remedies
Internal remedies:
Dashamula Kashayam – Decoction of 10 roots relieves pain, swelling and stiffness. The coarse powder of Dashamula is readily available in the Ayurveda herbal stores or pharmacies. 10 grams of the coarse powder is boiled with 160 ml of water until 40ml remains. The filtrate is taken hot. It is given 2-3 times in a day before food.
Devadaru Kashayam – Roots and bark of Devadaru (Cedrus deodara), 10 grams is boiled with 160ml of water until ¼ of it remains (40ml). The filtrate is taken hot, 2-3 times a day half an hour before food.
Erandamula Kashayam – Decoction of roots of castor plant is highly effective in osteoarthritis. It is prepared in the same way as mentioned in Dashamula Kashayam and taken in the same dose.
Castor oil – Edible castor oil in the dose of 10-25 ml (on the recommendation of Ayurvedic doctor) can be taken at bed time mixed with hot milk or with decoction of roots of castor plant.
Sesame – Take 1 tsp black sesame seeds and crush them. Dip them in 100ml of warm water and allow overnight. Mix them well and consume it first thing in the morning.
Cinnamon – Mix 1tsp cinnamon powder in 1 tsp honey. Take it on empty stomach every morning.
Asthishrunkala (Cissus quadrangularis) – Medicated ghee prepare with this drug is taken orally in doses of 10grams mixed in hot milk early in the morning. The juice of the plant can be given in 10ml dose with ghee in equal quantity. Macerated stem of the fresh plant is used for application over painful parts
Babul: Bark powder or seed powder of Babul is given in 3-5 grams dose with 1 spoon honey twice daily, half an hour after food
Lashunadi Kalka: Paste of equal parts of Garlic (paste of 2 cloves), Lac (2 grams approximately), honey (1 spoon) and sugar (1 spoon) is given mixed in ghee (1 spoon)
Arjuna twak churna: Powder of bark of Terminalia arjuna (3-5 grams) is given along with a cup of milk.
External remedies for osteo arthritis:
Apply required amounts of lukewarm castor oil or sesame oil on the afflicted joint and rub gently in clockwise direction for 10-15 minutes. Take a hot water bath after 1 hour. Alternately salt water fomentation (heat with cloth dipped in salt water) or fomentation with heated salt tied in a cloth relieves pain and swelling.
Add 5-10 grams of camphor to 1 cup of mustard oil. Heat the oil until camphor dissolves completely. Gently massage the joints with lukewarm oil. This reduces pain and inflammation and stiffness. It enhances blood supply to the joints.
Shatadhauta Ghrita: Ghee processed (washed) with medicinal herbs (their decoctions) for 100 times is mixed with Shali pishti (rice flour) and applied over the painful joints
Osteoarthritis modern perspective
Osteoarthritis – Disease review, Modern perspective
Causes and Risk Factors
The primary cause of OA is damage from mechanical stress with insufficient self repair by the joints. Sources of this stress are as mentioned below:
Misalignment of bones caused by congenital or pathogenic causes
Mechanical injury
Excess body weight
Loss of strength in the muscles supporting a joint
Impairment of peripheral nerves leading to sudden or uncoordinated movements
Exercise (including running in the absence of injury) and cracking the knuckles have not been found to be risk factors
Primary risk factors:
Hereditary basis – OA is found to have a greater prevalence among siblings and identical twins
Genetic factors – contributes towards variation in susceptibility towards OA
Sex – Women are more likely to develop OA
Age – Older age increases the OA
Evolution of human ancestors into bipeds led to changes in pelvis, hip joint and spine which led to increased risk of OA
History of previous joint injury and obesity (especially wrt knees) is a risk factor for OA. Correlation with obesity has been observed for other non-weight bearing joints also.
Changes in sex hormone levels (OA is more prevalent among post-menopausal women than among men of the same age). A study of mice found natural female hormones to be protective while injections of the male hormone dihydro-testosterone reduced protection.
Secondary Risk Factors:
This type of OA is caused by other factors but the resulting pathology is the same as for primary OA. They are:
Rheumatoid Arthritis – A chronic progressive disease causing inflammation in the joints and resulting in painful deformity and immobility, especially in the fingers, wrists, feet and ankles.
Read more: Diet for rheumatoid arthritis
Gout – A disease in which defective metabolism of uric acid causes arthritis, especially in the smaller bones of the feet, deposition of chalk-stones and episodes of acute pain.
Read related: Gout causes, treatment
Alkaptonuria – A rare recessive metabolic anomaly marked by ochronosis and presence of alkapton in the urine. (Ochronosis – accumulation of dark pigment in cartilage and other connective tissue, usually a symptom of alkaptonuria or phenol poisoning)
Congenital disorders of joints
Diabetes – It doubles the risk of having a joint replacement due to OA. People with Diabetes have joint replacements at a younger age than those without diabetes.
Read related: Ayurvedic treatment for diabetes
Ehlers-Danlos Syndrome – It is a group of disorders that affect the connective tissues that support the skin, bones, blood vessels and many other organs and tissues. Defects in connective tissues cause the signs and symptoms of EDS, which vary from mildly loose joints to life-threatening complications.
Haemochromatosis – It is a disease in which there is an excessive accumulation of iron in the body leading to iron overload.
Wilson’s disease – or hepatocellular degeneration is an autosomal recessive genetic disorder in which copper accumulates in the tissues, this manifest as neurological or psychiatric symptoms and liver disease.
Inflammatory diseases like Perthes’ disease (childhood disorder affecting the head of thigh bone in which the bone softens and breaks down due to inadequate blood supply), Lyme disease (infectious disease caused by bacteria of the Borrelia type) and other chronic forms of arthritis ex. rheumatoid arthritis and costochondritis gout are risk factors. In gout, uric acid crystals cause the cartilage to degenerate at a faster pace.
Injury to joints or ligaments as a result of an accident or orthopaedic operations and sports are risk factors for OA.
Bone deformities – malformed joints or defective cartilage from birth
Ligamentous deterioration or instability may be a factor
Marfan syndrome – It is a genetic disorder of connective tissue. It has a variable clinical presentation, ranging from mild to severe systemic disease. The most serious manifestations involve defects of the heart valves and aorta.
Obesity – Carrying excessive body weight contributes to OA in several ways. It puts added stress on weight-bearing joints such as hips and knees. In addition, fat tissue produces proteins that may cause harmful inflammation in and around your joints.
Certain occupations – Jobs including tasks that place repetitive stress on a particular joint
Joint infection
Signs and symptoms
Signs and Symptoms of Sandhivata – OA
Pain – generally described as a sharp ache or a burning sensation in the associated muscles and tendons. Joints may hurt during or after movements.
Tenderness – when light pressure is applied on the joint
Loss of ability to perform activities
Loss of flexibility – you may be unable to move your joint through its full range of motion
Stiffness – more prominent when you wake up in the morning or after a period of inactivity
Crackling noise (crepitus) / grating sensation when the joint is moved or touched
Muscle spasms and contractions in the tendons (experienced by patients)
Fluid in the joint (occasional) – OA is the most common cause of joint effusion of the knee
Increased pain associated with cold temperature, high humidity and / or a drop in barometric pressure (as reported by some patients
With progression – joints appear larger, stiff and painful. Patient feels better with gentle use but worse with excessive or prolonged use of joints (distinguishing feature from Rheumatoid Arthritis)
Nodes – In smaller joints such as at the fingers, hard bony enlargements called Heberden’s nodes (on the distal interphalangeal joints) and / or Bouchard’s nodes (on the proximal interphalengeal joints) may form. They may not be painful but can limit the movement of fingers significantly.
Bunions (Painful swelling of the first joint of the big toe) tenders the toes red or swollen
Bony spurs – extra bits of bone, which feel like hard lumps may form around your affected joint
Patho-physiology
OA is a degenerative joint disease. It causes gross cartilage loss and morphological damage to other tissues of the joints. In the earliest stages of OA progression we can find more subtle biochemical changes.
The water content of healthy cartilage is finely balanced by compressive force driving water out and swelling pressure drawing water in. Collagen fibers exert compression force forcing the water out. On the other hand, Gibbs-Donnan effect and cartilage proteoglycans create osmotic pressure which tends to draw water in. However, during onset of OA, the collagen matrix becomes more disorganized and there is a decrease in proteoglycan content within the cartilage. The breakdown of collagen fibers results in a net increase in water content. This increase occurs because while there is an overall loss of proteoglycans (and thus a decreased osmotic pull), it is outweighed by a loss of collagen. Without the protective effect of proteoglycans, the collagen fibers of the cartilage can become susceptible to degradation and thus exacerbate the degeneration.
Inflammation of the synovium (joint cavity lining) and the surrounding joint capsule can also occur. This can happen as breakdown products from the cartilage are released into the synovial space, and the cells lining the joint attempt to remove them.
Other structures within the joint can also be affected. The ligaments within the joint become thickened and fibrotic and the menisci can become damaged and wear away. Menisci can be completely absent by the time a person undergoes a joint replacement. New bone outgrowths called spurs or osteophytes can form on the margins of the joints, possibly in an attempt to improve the congruence of the articular cartilage surfaces in the absence of the menisci. The sub-chondral bone volume increases and becomes less mineralized (hypomineralization). All these changes can cause problems functioning. The pain in an OA joint has been related to thickened synovium and subchondral bone lesions.

Diagnosis
Diagnosis is chiefly based on history and clinical examination which almost provides the information of the existence of OA. X-rays may be used as a confirmative tool for diagnosis. Typical changes seen on X-ray include – joint space narrowing, subchondral sclerosis (increased bone formation around the joint)subchondral cyst formation and osteophytes. Usually other imaging techniques are not necessary to clinically diagnose OA.
Grading
Many classification systems are used for grading of OA. They are-
WOMAC scale
Kellgren-Lawrence grading scale
OA is classified as either primary or secondary depending on whether or not there is an identifiable cause
Primary OA can be sub-classified as primary generalized OA and erosive OA (EOA OR inflammatory OA)
Differential diagnosis
Differential Diagnosis of Osteoarthritis:
Bursitis – Greater trochanteric bursitis in the hip and pes anserine bursitis in the knee present with pain over the lateral aspect of the hip and over the medial aspect of the knee respectively. There is also local tenderness in these areas that is usually absent in simple OA.
Gout – Onset of arthritis in gout is usually more acute and over a period of a few hours, but could mimic an exacerbation of acute OA. Gout or pseudogout often co-exists in the same joint. In acute attacks, the affected joint is usually red, hot and tender. Gout commonly involves the foot, especially the first metatarsophalangeal (MTP) joint. It may affect almost any joint.
Rheumatoid Arthritis – RA usually causes a symmetrical small joint polyarthritis in the hands, particularly affecting the Metacarpo-Phalangeal joints. It spares the Distal Interphalangeal joints. Typically RA is associates with morning stiffness which is more prolonged than in OA. There is a feeling of being unwell associated with low mood and fatigue.
Psoriatic arthritis – It can occur in the presence or even absence of skin psoriasis. It often affects the Distal-interphalangeal joints. The joint involvement is usually asymmetrical.
Avascular Necrosis (AVN) – This is common in the hip and knee joints. The onset is subacute and there is usually a risk factor such as corticosteroid use. Early in the disease, the joint examination is unremarkable, except for possible localized bony tenderness in the knee.
Internal derangements (ex. meniscal tears) – The onset meniscal tears is usually acute and debilitating, with preceding trauma can be minor. Patients may describe true locking (normal flexion, but an inability to extend the affected knee).
Ayurvedic explanation Sandhigata Vata
Ayurvedic concept of Osteoarthritis –
Osteoarthritis is called Sandhigata Vata or Sandhi Vata in Ayurveda. Sandhigata Vata means a condition in which morbid Vata or Vayu is located in the joints and destroys the joints.
Nidana
What are the causes of Sandhigata Vata?
Since the disease is caused by vitiated Vata, all the foods, life activities which cause aggravation of Vata are the causes of Sandhigata Vata. Below mentioned are the causes of Vata Prakopa (vata vitiation) and hence causes of Sandhigata Vata vis-à-vis osteoarthritis.
Vata Prakopaka Karanani (Causative factors responsible for Vata vitiation):
- Vyayama – Excessive exercises
- Apatarpana – Fasting in excess
- Prapatana – Fall, injury
- Bhanga – Fractures
- Kshaya – Depletion of tissues
- Jaagarat – Excessive vigil (awakening all night)
- Veganam cha vidharanat – Suppression of natural body urges (reflexes)
- Ati shuchi – Excessive administration of cleansing procedures (Panchakarma)
- Shaityadi – Excessive consumption of cold foods and activities
- Traasaat – Fear
- Ruksha – Excessive consumption of dry foods
- Kshobha – Irritation
- Kashaya – Excessive consumption of astringent foods
- Tikta – Excessive consumption of bitter foods
- Katu – Excessive consumption of pungent foods
- Vari-ghanagame – cloudy and rainy season
- Parinate anne – After the digestion of food
- Aparahne – Evening
Among the causative factors for Asthivaha Sroto Dushti (Contamination of channels providing nutrition to bones and help in their formation) Vatala Ahara Vihara (Vata increasing food and activities) has been explained.
Samprapti
How does Sandhigata Vata occur?
Hanti sandhigataha sandheen shoola aatopau karoti cha (Ref-Madhava Nidanam, 22/21)
Vaata poorna druti sparshaha shothaha sandhi gate anile,
Prasaarana aakunchanayoho pravrittihi cha sa vedanaa (Ref-CharakaChikitsa 28/37)
The vitiated Vayu Dosha on getting lodged in the joints of the body, causes Sandhigata Vata
Signs and symptoms
The signs and symptoms of Sandhigata Vata are –
Shula (pain)
Atopa (abnormal sounds due to damage of joints or crepitus)
Vata purna driti sparsha – Sounds resembling that made when we rub against a balloon or transparent container filled with air
Shotha – Swelling
Prasarana Akunchanayoho pravritti savedana – Painful movement of the joints including extension and flexion.
Pathogenesis of Sandhivatam:
Vayu tends to pathologically increase in terms of quality and quantity when you consume vata vitiating foods and gets exposed to activities (physical and mental) which tend to aggravate Vata as mentioned above. This Vayu when gets vitiated beyond limitations (prakopa) tends to move all over the body in a haphazard and violent way (prasara). The vitiated vata can get lodged in any weak dhatu (tissue), impart pathological changes therein, damage the tissue and initiate a disease process (sthana samshraya). In case of Sandhigata Vata, the vitiated vayu gets lodged in weak asthi dhatu (bone tissue) and asthi-sandhi (bony joints). Asthi dhatu and Vata always are related to each other in an abode-resident (ashraya-ashrayi) relationship. Thus pathological increase or decrease of Vata has a serious impact and damaging effect on bone tissue more than any other tissue. Dhatu kshaya (depletion of tissues) is also a direct cause for aggravation of Vata. Thus in Sandhigata Vata there may be direct or indirect depletion of all the tissues, leading to deterioration in immunity and integrity of the body. When the vitiated vata damages the bones and joints considerably, the signs and symptoms (vyakta) of Sandhigata Vata like Shula (pain), atopa (crepitus, loose bodies) and shotha (swelling) are caused. If the condition is not taken care of even in this condition, many complications (bheda) like immobility, deformity, crippling etc are manifested.
Ayurvedic treatment
Treatment options for Sandhigata Vata vis-à-vis osteoarthritis in Ayurveda –
External treatments
Bahya Chikitsa (External treatment) –
Abhyanga (Therapeutic / Preventive Herbal Oil Massage) –
Abhyanga means performing a massage. Massage of the afflicted part or joint or joints in osteoarthritis, is done using herbal (medicated) oils. Medicated oil and mixture of medicated ghee is also preferred in some cases. Pain is generally caused due to aggravated Vayu / Vata. Taila (oil) is said to be the best remedy for vitiated Vayu. Massage not only alleviates the morbid Vayu but also provides significant relief from pain, swelling and catches. It nourishes and strengthens the bones, joints and soft tissues and also rejuvenates them. Abhyanga when performed as a daily practice keeps up the health of the joints while avoiding painful conditions even in the process of inevitable ageing. Ayurveda advocates whole body massage with herbal oils to be practiced on a daily basis.
Best oils used for Abhyanga:
- Tila Taila (Sesame oil)
- Ksheerabala Tailam
- Mahamasha Tailam
- Dhanwantaram Tailam
- Murivenna
- Pinda Tailam
- Mahanarayana Tailam
- Prabhanjana Vimardhana Tailam
- Kottamchukkadi Tailam
- Sahacharadi Tailam
- Yashtimadhu Tailam
- Guggulutiktakam Ghritam etc.
Swedana (Fomentation / Sudation / Sweating therapy) –
Sweda means sweating. Swedana means a treatment procedure in which sweating is induced. Swedana is usually done after Abhyanga and or Snehana (administration of medicated oils and ghee for oral consumption in metered doses, as a pre-treatment procedure for cleansing treatments like Vamana – Therapeutic vomiting and Virechana – Therapeutic purgation).
After Swedana, the cells get activated and flush the toxins away. The cellular metabolism improves and we feel light and at ease. Swedana done after abhyanga or snehana enables free circulation in the joints, removes pain, stiffness and swelling, strengthens and rejuvenates the joints, eases movements.
There are many types of Swedana as explained in Ayurvedic texts. But the below mentioned types of Swedana are generally practiced –
Bashpa Sweda –
Bashpa means steam, Sweda means sweating therapy. This type of fomentation includes giving steam to the whole body after having administered a whole body massage.
The below mentioned are the variants of Bashpa Sweda which can be effectively used for the relief of osteoarthritis –
Sarvanga Bashpa Sweda – This is a steaming treatment conducted so as to cover the whole body. This is done by making the patient (who has been given a massage) sit inside a steam-chamber keeping his head out of the box, through an opening given for that purpose. After proper steaming, the patient is let out of the steam chamber or cabin.
Ekanga Bashpa Sweda or Nadi Sweda – Ekanga means one region or part of the body. This type is meant for partial fomentation. When the pain is limited to a part of the body or when individual joints are afflicted with osteoarthritis, Ekanga Bashpa Sweda is preferred. This procedure is carried out by boiling pain alleviating drugs like Rasna, Eranda, Dashamula, Devadaru etc in a container with lid; say for example a pressure cooker. The nozzle of the cooker is connected with a heat resistant tube. When the contents in the vessel or cooker are boiled to optimum, the steam is released through the opening of the tube. The painful part or joint is exposed to the steam.
Pinda Sweda (Bolus Fomentation) –
Pinda means bolus, Sweda means inducing sweating. Thus in Pinda sweda, the medicaments, generally hot or boiled to tolerable temperature are tied in a cloth so as to make a bolus. The bolus is gently rubbed over the afflicted joints. Heat is provided until sweating occurs. Pinda sweda is generally done as a local fomentation, applied on the pain afflicted joints. There are many variants of Pinda sweda, the name is given on the basis of the material / medicaments tied within the bolus. The best Pinda sweda’s in business are mentioned below –
Churna Pinda Sweda (Podikkizhi) – Churna means herbal powder, Pinda means bolus, Sweda means fomentation. As the name indicates herbal powders are filled and tied in a sterile cloth so as to form a bolus. The powder is used either in dry form (high kapha-ama-meda conditions where rukshana or drying therapy is needed, presence of swelling and stiffness etc symptoms) or in wet form i.e. after frying the herbal powder in medicated oils (high vata-pitta conditions, presence of inflammatory and or degenerative changes, pain, burning sensation etc symptoms). The bolus is heated on a pan (dry fomentation) or dipped in pan consisting of oils (wet fomentation) before applying on the afflicted joints in OA and rubbing it. After heating, the bolus is brought in contact with painful joints and gently rubbed in circular motion over joints and vertically over the muscles. In osteoarthritis wet form (oil dipped) of churna pinda sweda is preferred as there is degeneration.
Note –
Ama means metabolic wastes created by low metabolism and indigestion which have a sticky nature and has a tendency to produce pain and stiffness.
Meda means fat.
Herbal powders used for Churna Pinda Sweda are:
- Rasnadi Churna,
- Ellumnishadi Churna,
- Grihadhoomadi Churna,
- Kolakulattadi Churna etc
Churna pinda sweda is done for 30-45 minutes
Patra Pinda Sweda (Leaf bolus fomentation) – Patra means leaves of medicinal plants, Pinda means bolus, Sweda means fomentation. As the name indicates sliced (chopped) leaves of medicinal plants having anti-inflammatory, anti-degenerative and analgesic properties are filled and tied in a sterile cloth so as to form a bolus.
The fresh leaves of the Vata alleviating / pain relieving herbs are collected and sliced. Ex. Leaves of Eranda (Ricinus communis – castor plant), Nirgundi (Vitex nigundo), Arka (Calotropis gigantean), etc are sliced. The sliced leaves are fried in herbal oil (oils used for Abhyanga). Grated coconut, sliced lemon, Rasnadi Churna, Haridra (Turmeric powder), Methika (fenugreek), Saindhava Lavana (rock salt), Eranda Taila (castor oil) are also added and fried. The sliced leaves are tied in a bolus to form a Patra Pinda (Leaf bolus). A couple of boluses are prepared
The leaf bolus is dipped in warm oil; temperature of the bolus is tested and used for giving fomentation. The bolus is rubbed on the affected part gently (as good as massaging with bolus). The procedure is repeated many times for a period of 30-40 minutes.
Shashtika Shali Pinda Sweda – Fomentation with Shashtika Rice (rice grown in 60 days duration) processed with medicinal decoctions packed in boluses shall be preferred when there are signs of severe Vata vitiation and degeneration of joints and tissues. The boluses are dipped in milk processed with pain alleviating decoctions and rubbed over the sore joints continuously for 30-45 minutes. It rejuvenates, nourishes and strengthens the bones, muscles and soft tissues.
Avagaha (Tub bath or Sitz bath) –
A big tub so as to accommodate the body of a person (like bathing tub) is filled with warm oils, ghee and oils, herbal decoctions and medicated (processed with medicinal drugs) milk. The patient who has joint pains due to osteoarthritis is given a massage and made to sit in the tub for 40-35 minutes. The temperature of the liquid medicines is kept constant by re-heating the medicine. This treatment alleviates inflammation, degeneration and stiffness associated with pain in the joints.
Dhara or Seka (Pizhichil) –
Dhara or Seka means to pour in streams. In this, medicaments including herbal oils and processed milk is poured in streams along with gentle stroking for a fixed duration. This is highly effective in combating morbid Vata, Pitta and Rakta in the sore joints.
Sthanika Vasti’s:
Kati Vasti –
Kati means Low back (Lumbo-sacral region), Vasti means pooling or holding any liquid / fluid in a restricted place within a compartment or cabin constructed in that region.
Thus Kati Vasti means a treatment in which pain relieving warm medicated oils are poured and pooled for a fixed duration of time in a compartment or a cabin constructed over the low back area using wet flour of black gram, covering the Lumbo-sacral and Sacro-iliac joints afflicted by OA.
In simple words, Kati Vasti is a pain relieving oil-pooling treatment conducted for low back pain caused due to many causes including OA
The temperature of the oil is kept constant. As the oil loses its temperature it is removed and replaced by warm oil. The procedure is carried out for 30-45 minutes. Kati Basti is a highly effective treatment for relieving back pain and discomfort caused due to OA. The constant contact of medicated oils with the afflicted area of the back helps in healing process. Kati Vasti combats not only pain but also catch, inflammation and degeneration effectively. It forms a highly effective combo with Pinda Sweda, especially Patra Pinda Sweda. Both are generally conducted together.
Janu Basti – Same as Kati Vasti, conducted over painful knee joints afflicted by OA. Read: Janubasti procedure, benefits
Greeva Basti – Same as Kati Vasti, conducted over painful nape of the neck afflicted by OA Read: Greeva Basti procedure, benefits
Prishta Vasti – Same as Kati Vasti, conducted over the whole spine afflicted by OA
Sandhi-Pichu –
A larger piece of cotton swab (pichu) is dipped in medicated oil and ghee, kept in the affected joint and bandaged. It is left in place for a prescribed duration before it is removed. This is carried on day to day basis. This will continuously keep nourishing the bones, joints and tissues, prevents degeneration, lessens inflammation, and heals pain and catches. The same oils used for Abhyanga can be skillfully used in this format of treatment also.
Sandhi Lepa –
Lepa means application. Powders of drugs which alleviate pain are made into paste. The paste is applied over the afflicted joints. It is allowed to stay in place for a prescribed period or till the paste starts to dry. Depending on the disease and dosha involved, the Lepa is applied either hot / warm (vata, kapha vitiation) or cold (pitta, rakta vitiation). The common medicines which are used for Lepa are –
Rasnadi Churnam
Kottamchukkadi Churnam
Grihadhoomadi Churnam
Ellumnishadi Churnam
Dashanga Lepam etc
Upanaha –
Upanaha means poultices. The same powders mentioned in lepa are used as medicaments in Upanaha. After mixing them with suitable medicated oils, salt etc.The medicines are applied and tied around the back such that the medicines lie in contact of the painful part for a prescribed duration until they are removed.
Internal treatments
Abhyantara Chikitsa (Internal treatment) for Sandhivayu –
This includes some of the Panchakarma (5 treatment procedures which are used in body cleansing / detoxification) treatment procedures which should be skillfully chosen as per the condition of the dosha and the diseased.
Snehapana –
Sneha means medicated oil or ghee, Pana means intake. Snehapana is a procedure in which the patient is made to drink metered doses of oil or ghee which are processed with medicines. This is given in 3 forms:
Shodana Sneha – Here the medicated ghee or oil is given in higher doses so as to cause saturation in the body. The dosage is increased every day until all the cells of the body get saturated or the symptoms of proper administration (Samyak Snigdha Lakshanas)of sneha are obtained or until the patient develops aversion towards the medicine. It is usually given early in the morning on empty stomach. It is given for patients for whom Shodana (body cleansing treatments like vamana – therapeutic emesis or virechana – therapeutic purgation) has been planned. After the body cells have been saturated with the Snehana, Swedana (whole body steaming) is given followed by administration of Vamana (therapeutic emesis) and or Virechana (Therapeutic purgation) is given.
Shamana Sneha – The same medicaments are given in smaller doses when the extent and strength of the disease and diseased are low or moderate. It is given when the patient feels hungry, before food. The intention is to pacify the vitiated Doshas and not to expel them.
Brumhana Sneha – The sneha is given for strengthening purposes and also for promoting bulk. The medicated oil or ghee is given mixed with food.
Nitya Snehapana – In this, small metered doses of Sneha is given on a daily basis either first thing in the morning or at bedtime usually mixed in hot milk or gruel. This method is followed when the patient is not able to take higher doses or is not fit for Panchakarma procedures. It acts as a lubricant and rejuvenates the joints and soft tissues. It also helps in tackling the morbid Vata and Pitta which are causing joint pains.
Important medicines used for Snehapana in Sandhivata –
- Guggulutiktakam Ghritam
- Tiktakam Ghritam
- Indukantham Ghritam
- Bala Tailam
- Rasnadi Ghritam
- Mahamasha Tailam
- Brihat Chagaladya Ghritam
- Amritaprasha Ghritam etc.
Virechana in Sandhigat Vata (OA)
Virechana means therapeutic purgation. Virechana is given after the administration of Snehapana and Swedana. Virechana expels the morbid dosha’s especially pitta and vata, thus preventing or curing the osteoarthritis.
Nitya virechana – This is a variant of Virechana where in the medicines which have a laxative property are given in low doses on a daily basis. This will target expulsion of morbid doshas on a daily basis, as and when they are formed and tending to cause some pathological changes in the low back area. Apart from expelling morbid vata and pitta, it also relieves pain, inflammation and stiffness of the degenerating joints.
Best medicines used for Virechana (depending on the morbid dosha and morbidity):
- Gandharvahastadi Kashayam
- Gandharvahastadi Eranda Tailam
- Nimbamritadi Eranda Tailam
- Higutriguna Tailam
- Shaddharana churnam
- Trivrit Leha
- Sukumara Leha
- Kalyana Gulam
- Sukumara Ghritam
- Sukumaram Kashayam
- Hingutriguna leham
- Triphala Churnam
- Narayana churnam etc
Vasti treatment for Sandhivatam:
Vasti means medicated enemas. Vasti or Basti is said to be the best treatment for vitiated Vayu, which is the chief culprit in pain games. When Vayu is controlled by the action of Vasti all the other disturbed body elements fall into rhythm and equilibrium. Vasti strengthens the joints and soft tissues, rejuvenates health, aids fast healing and prevents recurrence.
Many times, constipation and accumulation of gases in the belly is the cause for joint pain. Virechana and Vasti act as effective purgatives and relieve the mentioned conditions.
Vasti is given in the below mentioned forms:
Asthapana Vasti (Kashaya Vasti) – Herbal decoctions or milk (ksheera vasti) processed with decoctions is given as enemas.
Below mentioned are some of the best Asthapana Vasti’s in osteoarthritis –
Erandamuladi Kashaya Vasti
Dashamula Kashaya Vasti
Dashamula Ksheera Vasti
Mustadi Yapana Vasti etc.
Anuvasana Vasti – Medicated oils or ghee is used for enemas. It is given in combination with Asthapana Vasti (alternatively).
Matra Vasti – It is also a variant of Anuvasana Vasti but given in small doses. It can be given on a daily basis until the back related problems get resolved. Matra vasti lubricates the joints and relieves pain and associated conditions.
Best medicines used for Anuvasana and Matra Vasti for Sandhi vata are –
- Guggulutiktakam Ghritam
- Tiktakam Ghritam
- Ksheerabala Tailam
- Mahamasha Tailam
- Sahacharadi Tailam
- Brihat Saindhavadya Tailam
- Bala Tailam etc.
Udwarthana – It is a treatment in which herbal powders either mixed or not mixed with medicated oils are rubbed against the body in an upward direction. It is a popular treatment and is an essential part of weight reduction and anti-obesity treatment packages. The treatment is said to mobilize and expel morbid kapha and meda (fat) responsible for causing blocks in the transport systems of the body. It is not a direct treatment for osteoarthritis. Udwarthana helps because by eliminating morbid kapha and meda, it relieves the stress of body weight over the joints. Overweight and obesity are risk factors for joint pains and osteoarthritis, especially OA of knee joints and low back joints.
Tikta Ghrita – Ghee processed with decoction of bitter drugs shall be used for drinking purpose and also for enemas
Treating Vayu in sandhivata:
- Sneha – Administration of medicated oils / ghee, Massage, oil pouring etc
- Sweda – Steaming / sudation / sweating therapy
- Mridu shodanam – Evacuation treatment (mild cleansing treatments like Virechana etc)
- Svadu bhojana – Consuming sweet foods
- Amla bhojana – consuming sour foods
- Lavana bhojana – consuming salt foods
- Ushna bhojana – Hot and fresh foods
- Abhyangam – Massage with herbal oils
- Mardana – Tapping the body with closed fists after application of vata alleviating oils
- Seka – Pouring of medicated oils over the body in streams
- Paishtika Madhya – Alcohol or fermented products prepared with flours
- Goudika Madhya – Alcohol or fermented products prepared with jaggery
- Snigdhoshna Vasti – Medicated enemas with oils and ghee, given luke warm
- Deepana pachana sneha – Oils and ghee processed with deepana (appetizer) and pachana (digestant) drugs
Prevention of Sandhigata Vata – Sandhigata Vata vis-à-vis osteoarthritis can be prevented by avoiding food and life style activities which aggravate Vata (explained above)
Correction of Agni
Correction of Agni, Ajeerna and Ama in Sandhi Vata:
Disturbance of metabolism, indigestion and metabolites are said to be the initial culprits (culprits at the foundation) of osteoarthritis.
Loss of appetite, indigestion and any symptom related to upper or lower gastro-intestinal tract persisting for a longer duration should not be taken lightly.
They should be corrected by administration ghee processed with deepana (fire stimulating or appetizing) drugs and pachana (digestion promoting or ama destroying) drugs or the same drugs mixed in ghee. Medicines can be given in other forms also – Churna, Kashayam, etc
Ex: Ardhraka Ghrita, Guggulutiktakam Ghritam / Kashayam, Tiktaka Ghritam / Kashayam, Pippalyadi Ghritam, Indukantam Ghritam, Trikatu Churna, Panchakola churna etc.
The same medications correct errors of dhatugata agnimandhya (low tissue metabolism) and strengthen the tissues, the medo dhatvagni and asthi dhatvagni in this case.
Medo chikitsa
Medo-chikitsa / Medoroga chikitsa in Sandhivat
Since Meda or fat is the immediate precursor of Asthi dhatu, treatment and medications to prevent or reduce accumulation of fat in the body should be administered, especially if the patient has a weight putting tendency or is obese.
Virechana (Therapeutic purgation), Lekhana Vasti (fat eliminating enemas) and Udwarthana (massage done with herbal powders in the reverse direction) would provide benefit in these cases.
Anti-obesity medications should be given to reduce weight and fat. Ex: Medohara vidangadi lauha, Navaka Guggulu, Varadi Kashayam, Varanadi Kashayam, Guggulutiktakam Kashayam etc.
Guggulu (Commiphora mukul) preparations
Lakshadi Guggulu
Aabhadi Guggulu
Ayurvedic medicines, herbs
Best formulations for osteoporosis:
- Maharasnadi Kashayam
- Dhanwantaram Kashayam
- Ashwagandharishtam
- Dashamoolarishtam
- Balarishtam
- Aabhadi Guggulu
- Lakshadi Guggulu
- Trayodashanga Guggulu
- Yogaraja Guggulu
- Medohara Vidangadi Lauha
- Navaka Guggulu
- Shallaki
- Vatagajankusha Rasa
- Vata vidhwamsini Rasa
- Tiktaka Ghritam
- Guggulutiktaka Ghritam
- Shatavari Ghritam
- Ashwagandhadi Ghritam
- Mukta shukti Bhasma / Mukta shukti pishti – Pearl calcium
- Mukta Bhasma / Mukta pishti
- Shringa Bhasma
- Akik pishti
- Gandha Tailam
- Ksheerabala tailam 101
- Dhanwantaram 101
Yogas from Sahasra Yoga Text book
- Panchatiktaka guggulu gritha
- Rasna Sunthyadi Kashaya
- Karaskara Ghrita
Important drugs used for treating osteopenia:
- Guggulu – Commiphora mukul
- Shallaki – Boswellia serrata
- Haridra – Curcuma longa
- Ashwagandha – Withania somnifera
- Shunti – Zingiber officinale
- Dashamula – 10 roots
- Asthishrunkala – Cissus quadrangularis
- Amalaki – Emblica officinalis
- Arjuna – Terminalia arjuna
- Equisetum arvense – Horsetail
- Laksha – Lac
- Triphala – Fruits of Terminalia chebula, Terminalia bellirica and Emblica officinalis
- Pravala – Coral
- Tila – Sesame seeds
- Babul – Vachellia nilotica / Acacia nilotica
- Shigru – Moringa oleifera (drumstick)
- Nagabala – Grewia hirsute
- Shatavari – Asparagus racemosus
- Kumari – Aloe vera
- Shatavari – Asparagus racemosus
- Sahachara – Strobilanthes heynianus
- Bala – Sida cordifolia
- Devadaru – Cedrus deodara
- Eranda – Ricinus communis
- Rasna – Pluchea lanceolata
Modern management
Management of Osteoarthritis, Modern perspective –
Weight loss (for overweight people)
Exercises – moderate exercise will help in OA of hip and knee. These exercises should be done at least thrice weekly.
Massage therapy – This surely helps in improvising the symptoms of OA and enables free movements
Manual Therapies – It is also called as manipulative therapy. It is a physical treatment primarily used by massage therapists, physiotherapists, occupational therapists, chiropractors, osteopaths and osteopathic physicians to treat musculoskeletal pain and disability. It commonly includes kneading and manipulation of muscles, joint mobilization and joint manipulation.
The 3 important forms of manual therapy are:
Manipulation – it is an artful introduction of a rapid rotational, shear or distraction force into an articulation. It is often associated with an audible popping sound caused by the instantaneous breakdown of gas bubbles that form during joint cavitation.
Mobilization – is a slower, more controlled process of articular and soft-tissue (myofascial) stretching intended to improve bio-mechanical elasticity.
Massage – is typically the repetitive rubbing, stripping or kneading of myofascial tissues to principally improve interstitial fluid dynamics
Functional, gait and balance training – to improvise impairments of position sense, balance and strength in individuals with lower extremity arthritis as these can contribute to higher falls in older individuals
Knee braces – may help in knee OA
Heat applications – relieves stiffness of joints in OA
Cold applications – can relieve muscle spasms and pain in OA
Surgery –
Joint replacement surgery or resurfacing – recommended if problems are significant and more conservative management is ineffective. Joint replacement for both knee and hip joints are clinically effective and cost-effective.
Transfer of articular cartilage from a non-weight bearing area to the damaged area is an option but it may be a failure when the transferred cartilage does not integrate well with the existing cartilage at the transfer site.
Osteotomy – may be useful for some patients of OA
Arthroscopic surgery is not recommended due to poor outcomes and harmful effects
Alternative medicine –
The below mentioned options have been tried in OA management with varying effects and results:
- Glucosamine sulphate and glucosamine hydrochloride (glucosamine is a precursor for a component of cartilage)
- Phytodolor, SAMe and SKI 306X (Chinese herbal mixture)
- Cat’s claw
- Symphytum officinale – Comfrey roots
- Angelica archangelica – Wild celery / Holy Ghost
- Avocado/Soybean unsaponifiables (ASU)
- Methylsulfonylmethane
- Rose hip
- Boswella serrata
- Collagen
- Devil’s claw
- Duhuo Jisheng Wan (Chinese herbal preparation)
- Fish liver oil
- Ginger
- Herbal preparation Gitadyl
- Hyaluronic acid
- Omega-3 fatty acids
- Stinging nettle
- Turmeric
- Vitamins A, C and E in combination, Vitamin E alone, Vitamin K and willow bark
- Acupuncture
- Electro-stimulation techniques like TENS
- Low level laser therapy
- Tai Chi and Yoga – These are movement therapies involving gentle exercises and stretches combined with deep breathing. Some studies have shown that Tai Chi and Yoga when practiced regularly reduces pain associated with OA.
Researches
Data from first National Health and Nutrition Examination Survey (NHANES) – a programme of studies designed to assess the health and nutrition of Americans showed that obese women were nearly four times as likely as non-obese women to have OA. The risk for obese men was nearly 5 times greater than for non-obese men.
In a study of OA in a population in Framingham Mass, researchers estimated that overweight women who lost 11 pounds or about 2 body mass index (BMI) points, decreased their risk of OA by more than 50% while a comparable weight gain was associated with an increased risk of later developing knee OA. Read related
Researches show that if the muscles that run along the front of the thigh are weak, you have an increased risk of painful knee OA. Even relatively minor increases in the strength of these muscles, the quadriceps, can reduce the risk.
A long-term study of 1.321 graduates of Johns Hopkins Medical School found that people who injured a knee in adolescence or young adulthood were 3 times more likely to develop OA in that knee compared to those who had not suffered an injury. People who injured their knee as an adult had a 5 times greater risk of OA in the joint.
Framingham study found that moderate intake of vitamin C (120-200 mg/day) reduced the risk of OA progression by 3 times.
Framingham study showed that people who have knee OA and low blood levels of vitamin D are 3 times more likely to experience the disease progression, compared with people with high levels of the vitamin.
Latest research suggests that Diabetes Mellitus which affects the body’s ability to regulate blood sugar (glucose) may be a significant risk factor for OA. That’s because high glucose levels speed the formation of certain molecules that make cartilage stiffer and more sensitive to mechanical stress. This connection between diabetes and joint damage may help explain why more than half Americans diagnosed with DM also have arthritis.
According to a recent English study, those who regularly consumed non-citrus fruits like berries, apples, plums and peaches containing antioxidants were found to have less development of OA in comparison to those who didn’t.
A study in King’s college London in 2010 showed that Diallyl sulphides, the compounds known as alliums found in garlic, onions and leeks inhibited the enzymes that cause joints to degenerate
Ginger alleviated muscle pain for up to 24 hours after intense exercise and reduced joint inflammation (Research – University of Georgia)
Sprifermin and Strontium ranelate have been tried to see if they can modify outcomes in OA
Neurological, mechanical and imaging markers of OA risk – In OA, changes may occur before clinical disease is evident. This happens due to abnormalities in biomechanics, biology and structure of joints that predispose them to develop clinical disease. Research works are focused on defining these early pre-OA changes using the above mentioned markers of OA risk emphasizing multi-disciplinary approaches and looking into personalized interventions that can reverse OA risk in healthy joints before the disease becomes evident.
Gene transfer strategies – target the disease process rather than the symptoms of OA
Biomarkers –
Biomarkers for OA looking for molecules that could be used for risk assessments found 37 different biochemical markers of bone and cartilage turnover in 25 publications published in 2015. Some of them are –
Urinary C-terminal telopeptide of collagen type II (uCTX-II) – for knee OA progression
Serum cartilage oligomeric protein (COMP) levels – for incidence of both knee and hip OA, uCTXII is also identified as a biomarker in hip OA
Studies –
In 1990, the American College of Rheumatology developed criteria for the diagnosis of hand OA based on enlargement of hard tissue and swelling of certain joints. These criteria were found to be 92% sensitive and 98% specific for hand OA versus other entities such as Rheumatoid arthritis and spondyloarthropathies.
History, Epidemiology
History –
Evidence for OA found in the fossil record is studied by paleopathologists, specialists in ancient disease and injury. OA has been reported in fossils of the large carnivorous dinosaur Allosaurus fragilis.
Epidemiology –
OA is the most common form of arthritis with disease of the knee and hip affecting about 3.8% of people
Globally approximately 3.6% of population (250 million people) have OA knee
It is the cause of about 2% of years lived with disability
Just before finishing,
Osteoarthritis is very common disease of joints which holds the privilege of being a part of almost every family, afflicting at least one or two people of the family. It not only cripples the life of the person suffering from it but also disturbs the life of everyone related to him or her. It is going to haunt almost each one of us as we head towards ageing process. Prevention becomes the key to get over OA.
I hope that this article has given you an idea and insight of what Ayurvedic science offers towards better management and prevention of Osteoarthritis. The treatments mentioned above can help in preventing as well as curing osteoarthritis effectively. You can definitely tackle OA even before it manifests but before that it is wise to take an opinion of your Ayurvedic doctor so as to which treatment or medicines suits you the best.
Click to Consult Dr Raghuram Y.S. MD (Ayu)







11 comments
Gita
Excellent in depth informative article!
DR P JAFFAR ALI KHAN
Very informative article very useful to the patients and general public.
Sunil
Dear Dr Hebbar,
Excellent article. Is there an ayurveda treatment for avascular necrosis of femoral head ? Doctors mostly suggest Hip replacement as the only option.
Dr J V Hebbar MD(Ayu)Author
I have tried to treat it but without any success thus far. If you wish to try, please write to me here – [email protected]
Parimala Muniandy
hie just wanted to ask – can the knee cartilage be repaired & get it formed back to it’s natural state through any consumption (oral,internally) ? do let me know..
Natubhai
No article I have ever read is found so full of useful details.This is a great contribution to
‘Sandhivaat patients’. Thanks for this great humane service.
Vidya
Very useful sir !
Thank you very much for compiling this informative article!
Dr J V Hebbar MD(Ayu)Author
Welcome 🙂
Rajan
Dear Dr., kindly let me know what type of food to be avoided for osteoarthritis (hip, lower back, knee, shoulder pain)
Dr J V Hebbar MD(Ayu)Author
Avoid excess spicy foods, chillies, junk food, aerated drinks, smoking and alcohol.
Neil McDermott
Namaste Dr,
What a presentation I’m very humbled by the detail you presented and I guess as a patient one gleans what is important to us individually from this presentation which is Universal in its application.
For me at 72 years old it’s very connectable with in all aspects, Im grateful to to the Lord for a Pitta Kapha body and mind but the Kapha can rule so easily by “taking it easy”.The recommendations suggested are soo useful and clear even a few exercises, food recommendations are great to hear.