Low Bone Density Causes, Ayurvedic Treatment, Diet
By Dr Raghuram Y.S. MD (Ay)
Brittle bones can break even without a fall. This can happen due to low bone density and less minerals in bones. It is called Osteopenia.
Table of Contents
What is Osteopenia?
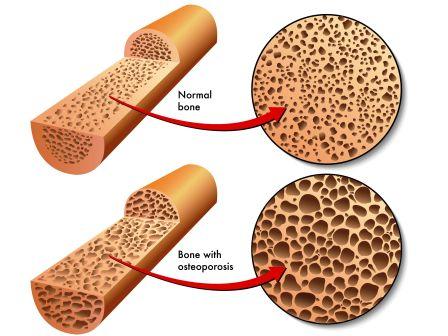
Osteopenia is a condition in which your bone density is lower than normal peak density. It leads to bone weakening and an increased risk of bone fracture. But the density is not low enough to be classified as Osteoporosis.
Osteoporosis is an advanced condition of Osteopenia in which the bone density is even low, much lesser than in Osteopenia.
It is defined as a bone mineral density with T-score between -1.0 and -2.5

Low bone density prevention
How to prevent low bone density?
As per Ayurveda to have good bone health, one should consume good amounts of oils (sesame oil, olive oil) and ghee.
Oil massage, at least once a week with sesame oil or Ayurvedic oils such as Mahanarayana oil is highly recommended.
Consume calcium sources:
Calcium is the most important mineral for the maintenance of bone mass. The best sources of calcium are –
- Milk and other dairy products
- Green vegetables
- Calcium-enriched products
Calcium supplements – Calcium tablets often combined with Vitamin D are prescribed in osteopenia.
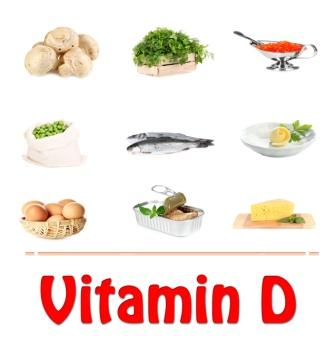
Vitamin D:
- It helps your body to absorb calcium and other minerals
- It is found in eggs, salmon, sardines, swordfish and some fish oils
- It is added to milk and can be taken instead of calcium and vitamin supplements
- Body makes natural vitamin D when it is exposed to sunlight
Exercise:
It is important for having strong bones. Bone forms in the body in response from stress. Weight-bearing exercises which exerts stress on bones like walking, hiking and dancing are all good choices. Adding exercise with light weights or elastic bands can help the bones in the upper body. Talk to your doctor or a physical therapist about starting an exercise programme.
Quit smoking
Avoid excessive use of alcohol and beverages like cola
How to maximise bone density?
- Sun-time – Spend some time walking or jogging in the sun, early in the morning
- Include – Calcium and vitamin D in diet
- Exercise – Get into weight bearing exercises regularly
- Avoid smoking, aerated drinks, sodas, excessive alcohol.
Plant oestrogen: Good for women especially for those around menopause
- Soybean
- Lentils
- Chickpeas
- Beans

Good foods for bones
Calcium requirement:
- Adults up to age 50 – up to 1,000 mg / day
- Beginning at age 51 – women needs 1,200 mg / day (men at and from 71 years of age)
Milk: Milk is the rich source of calcium. It is said to be pop star of calcium sources. A single 8 ounce cup of milk (skim or low-fat or whole) supplies you a serving of 300 mg of calcium.
Yogurt and Cheese: A cup of yogurt has at least as much calcium as an 8-ounce cup of milk
Sardines (Small fatty fish usually canned) –3 ounces of canned sardines gives you a little more calcium than a cup of milk.
Greens: Dark leafy greens, bok choy, Chinese cabbage and Kale, collard, turnips.
Oatmeal, soy food, calcium enriched tofu,
Salmon, fatty fishes contain Vitamin D, Omega-3 fatty acids.
- Salmon and other fatty fishes offer bulk of bone-boosting and strengthening nutrients. They contain vitamin D. They are also rich in omega-3 fatty acids. These constituents help bones. Fish oil supplements reduce bone loss in women and may help in preventing osteoporosis.
Nuts and Seeds:
- Walnuts and flaxseeds are packed with omega-3 fatty acids.
- Peanuts and almonds contain potassium which protects against the loss of calcium in urine
- Nuts also contain protein and other nutrients that play a supportive role in building strong bones
- Hazelnuts
Restrict Salt:
- Salt deprives the calcium contents of the body.
- The more salt you eat, the more calcium gets carried away from your urine.
- Stick to a low-salt diet. This will help conserve calcium in your body and strengthen your bones.
Other foods:
- Whole grains
- Broccoli
- Brussels
- Cabbage
- Sprouts
- Beans
- Black gram
- Chickpeas
- Green gram
- Seaweeds
- Honey
Others:
Sun-Shine:
- Body produces vitamin D in response to sunlight.
- Without vitamin D, our bodies cannot properly absorb the calcium in our foods.
- Interfering factors – Cloudy weather, northern latitude and darker skin
- Recommended dietary intake of vitamin D is 600IU for most adults (over 800IU above 70 years of age)
Weight bearing exercises
- Regular weight bearing exercises will help you to get most of your bone-boosting diet.
- This includes any activity that uses the weight of your body or outside weights to stress the bones and muscles
- As a result of this – the body lays down more bone material, your bone becomes stronger
- Brisk walking, dancing, tennis and Yoga – benefit your bones
Calcium supplements
- Should be considered if you don’t get enough calcium from your diet
- Take no more than 500 mgs at one time (take doctor’s opinion)
- Supplements like calcium carbonate are better absorbed if taken with food; calcium citrate can be taken anytime
Note: If you get enough calcium from food, taking pills too can increase side effects of excess calcium like kidney stones etc.
Try at home:
- Dandelion tea
- Almond milk (soak almonds in water and then add them in milk or soya milk)
- Dairy products, mainly milk
- Plenty of soy products
- Eat more pineapples, spinach, whole wheat and beans
- Eat chaste berry
- 1 teaspoon of honey everyday
- Handful of sesame seeds early in the morning
- Green tea
How much vitamin D and calcium do we need?
Ref: Institute of Medicine
http://www.webmd.com/osteoporosis/features/are-you-getting-enough-vitamin-d-calcium
Vitamin D
- Adults of age group 19-70 years of age – 600IU /day
- Adults older than 70 years of age – 800IU/day
Calcium
Daily requirement varies with age and gender:
- Newborns to 6 months – 200 mg
- Babies 7-12 months – 260 mg
- Kids, 1-3 years – 700 mg
- Kids, 4-8 years – 1,000 mg
- Kids and teens, 9-18 years – 1,300 mg
- Adults, 19-50 years – 1,000 mg
- Adult men, 51-70 years – 1,000 mg
- Adult women, 51-70 years – 1,200 mg
- All adults, 71 years and older – 1,200 mg
- Pregnant / Breastfeeding women – 1,000 mg
- Pregnant teens – 1,300 mg
Other foods which have vitamin D are:
- Salmons and sardines, egg yolks, Tuna, Mackerel, Shrimp, Mushrooms
- Foods with added vitamin D, such as milk, cereals, yogurts and orange juices
- Cod and fish liver oils
Should I get my Vitamin D blood test done?
- Some doctors prefer checking vitamin D levels, some don’t.
- If you are concerned that you might be running low vitamin D, you can ask your doctor to get your blood values checked
- People with certain health conditions like inflammatory bowel disease are at a higher risk for having vitamin D
- Those who don’t go out of home (outdoors) much, have darker skin, don’t take supplements and don’t eat foods rich in vitamin D are at a higher risk for having low vitamin D
- Your doctor may prescribe supplements if your blood shows low level of vitamin D
Follow up:
- Repeat BMD, usually after 2 years to detect progressive bone loss and determine if treatment is needed (when medication has not been started)
- A follow up test for BMD is frequently repeated after treatment with prescription is begun.
Why is osteopenia important?
- Osteopenia is important because it can cause bone fractures
- People with osteopenia are not as likely to fracture a bone as those with osteoporosis
- But in comparison to osteoporosis, there are many people with osteopenia. Obviously patients with osteopenia account for a large number of patients who fracture a bone.
- Remember – People with osteoporosis have greater risk of fracturing a bone than those with osteopenia
- Bone fractures due to osteopenia and osteoporosis are important because they can be very painful although some spinal (vertebral) fractures are painless
- Hip fractures not only cause pain but also require surgical repair
- Many patients require a long-term nursing home care after a hip fracture. Fractures in elderly are associated with an increase in overall mortality (death rate). Many people die in a short period following hip fracture due to complications including blood clots related to immobility, pneumonia and many other reasons.
Osteopenia causes
Calcium is absorbed into the body and in some circumstances, bone loses some part of calcium from it (called bone re-absorption).
As people grow older, the bones naturally become thinner. The changes start to happen in middle age itself. There should always be a balance between bone formation and bone re-absorption by the body which is quiet normal before we attain middle age, i.e. during active growth. After middle age, the more of the existing bone cells are reabsorbed by the body in comparison to the new bone being made. This means to tell that as we age further, the bone formation will become less in comparison to bone re-absorption.
As this occurs, the bones lose minerals, heaviness (mass) and structure (shape and size). This further makes the bones weaker. This also increases their risk of breaking.
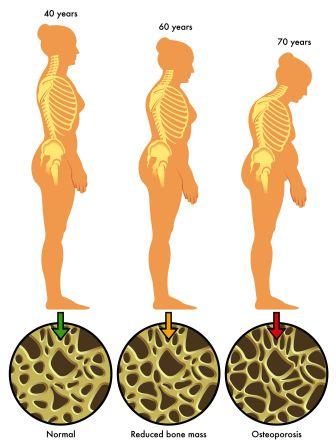
All of us reach the peak of bone density at about 30 years of age. After this people begin losing bone mass. The thicker your bones are at about age 30, the longer it takes to develop osteopenia and /or osteoporosis.
Osteopenia may be a result of one or more other conditions, disease processes or treatments.
Causes:
Osteopenia occurs more frequently in post-menopausal women due to loss of oestrogen
Women are more likely to develop osteopenia and osteoporosis than men.
The reason is that:
- Women have a lower peak bone density
- Hormonal changes during menopause speeds up the loss of bone mass
Other important causes for osteopenia:
- Genetics (family disposition to osteopenia and / or osteoporosis, family history of early bones and other genetic disorders)
- Hormonal (decreased oestrogen as in women after menopause or testosterone in men)
- Eating disorders and metabolism problems that do not allow the body to take in and use enough minerals and vitamins
- Chemotherapy or certain medicines (ex. corticosteroids and anti-seizure medications)
- Mal-absorption due to conditions like celiac sprue
- Chronic inflammation due to medical conditions such as Rheumatoid arthritis
- Exposure to radiation
- Being thin (Thin frame of body)
- Being white or Asian
- Limited or less physical activity (Immobility)
- Smoking
- Excessive beverage drinks
- Excessive alcohol
Exacerbating factors
- Lack of exercise
- Excess consumption of alcohol
- Smoking
- Prolonged use of glucocorticoid medications
- Exposure to radiation
More frequently in –
- Participants in non-weight-bearing sports like bicycling or swimming than in weight-bearing sports like running
- The condition is often noted in young female athletes. It is one of the 3 major components of female athlete triad syndrome along with amenorrhoea and disordered eating. Female athletes tend to have lower body weight, lower fat percentage and higher incidence of asthma than their less active peers. A chronic energy balance can suppress oestrogen levels and decrease bone mineral density
- It is also a sign of ageing, in contrast to osteoporosis which is present in pathological ageing
- Osteopenia is also a common effect of celiac disease
Symptoms
- Even as the bone becomes thinner and start losing density you may not notice pain or any other changes
- The risk of breaking a bone increases as the bone becomes less dense
Diagnosis
Osteopenia is diagnosed with a ‘Bone Density Test’
Dual-energy X-ray absorpimetry (DXA) –
It is the most accurate test of bone density
It is a form of X-ray which detects as little as 2% of bone loss per year
A DXA scan measures Bone mineral density (BMD) in the hip, spine and sometimes wrists. These locations are chosen because these are frequent sites of bone fracture.
Standard X-ray is not diagnostic of osteopenia (not sensitive to detect small amounts of bone loss or minor changes in bone density)
USPSTF (United States Preventive Services Task Force) recommends that all women around 65 years of age and older should have a bone density test to screen for osteoporosis. It recommends that you and your doctor check fracture risk using a tool such as FRAX. FRAX will help to decide whether you should be screened for osteoporosis.
FRAX tool was developed by the World Health Organization (WHO) to predict your risk of having a fracture related to osteoporosis in the next 10 years.
Other tests:
- Peripheral X-ray absorptiometry (pDXA)
- Quantitative computed tomography (QCT)
- Peripheral QCT (pQCT)
- Quantitative ultrasound densitometry (QUS)
How to do?
- You too can use FRAX
- Go to the website at sheffield.ac.uk/FRAX
- Click on Calculation Tool
- This will help you if you have had a bone density test on your hip
- If you have undergone this test, type in your score
- If you have not undergone the test, leave the score blank
Who should be tested for osteopenia?
Everyone doesn’t need to undergo a Bone Mineral Density test. Your doctor is the right person to decide if you need to undergo the test after a preliminary set of tests and examinations. The National Osteoporosis Foundation recommends the following groups of people be tested for osteopenia (or osteoporosis):
- Women 65 years and older, men 70 years and older
- Post-menopausal women and men 50-69 years of age at increased risk of osteoporosis
- Adults who have a bone fracture after age 50
- Adults with a medical condition associated with bone loss (such as rheumatoid arthritis) or who take a medication which can cause bone loss (prednisone or other steroids)
- Anyone being considered for prescription treatment for osteopenia or osteoporosis
- Anyone being treated for osteoporosis to monitor treatment
Risk Factors
- Being white (Caucasian) or an Asian
- Family history of Osteoporosis
- Being thin
- Long-term use of
- Corticosteroids, such as hydrocortisone or prednisolone for inflammatory conditions
- Anticonvulsants such as carbamazepine, gabapentin
- Phenytoin for pain or seizures
- Eating disorders or diseases that affect the absorption of nutrients from food
- Being inactive or bedridden for a longer duration of time
- Smoking
- Drinking excessive alcohol
- Having a diet low in calcium or vitamin D
- Men with low levels of testosterone also are at a risk of developing osteopenia
Allopathic treatment for low bone density:
Treatment should aim at taking steps to prevent osteopenia from progressing towards osteoporosis
Treatment of osteopenia includes –
Lifestyle changes that can help reduce bone loss
Medicines for diagnosed osteopenia
Therapy recommendations (medicines) –
https://en.wikipedia.org/wiki/Osteopenia
Target group – Those at highest risk of osteoporotic bone fracture based on BMD and clinical risk factors
As of 2008 recommendations from National Osteoporosis Foundation (NOF) are based on risk assessments from WHO Fracture Risk Assessment Tool (FRAX). According to these recommendations, therapy should be considered for postmenopausal women and men older than 50 years of age if any one of the following is present:
- Prior hip or vertebral fracture
- T-score of -2.5 at the femoral neck or spine, excluding secondary causes
- T-score between -1.0 and -2.5 at the femoral neck or spine and a 10-year probability of hip fracture ? 20%
- Clinicians’ judgement in combination with patient preference indicates treatment for people with 10-year fracture possibilities above or below these levels.
(Notably the first 2 conditions identify individuals with osteoporosis. The 3rd condition corresponds to individuals with osteopenia, namely those with T-score between -1.0 and -2.5)
Prognosis
- Bone loss can be slowed or stabilized with lifestyle changes or medication if necessary.
- In some situations, bone loss may continue due to hormonal factors, medical conditions or medications. Ex. untreated celiac sprue, untreated or resistant rheumatoid arthritis and treatment with steroid medication such as prednisone used for another medical condition
Prevention
The below said things determine that you have a tendency to develop osteopenia –
- Family history of osteopenia or osteoporosis
- Taking steroids for chronic asthma
- Quantity of calcium and vitamin D which you have taken (for your deficiencies) while you were growing up
- There is nothing much you can do about it
You can develop strong bones and help slow down osteopenia and prevent osteoporosis by taking appropriate measures if:
- You are a young adult
- You are raising children
Best before 30:
- Any measures taken to increase bone density and prevent osteopenia and osteoporosis will have long-term benefits if they are brought into practice before you have reached 30 years of age. This is because your bones don’t reach their greatest density until you are about 30 years of age. Therefore preventive measures best fit to children and youngsters below 30 years of age.
Differential Diagnosis
Osteoporosis –
Cause – Reduction in bone mass density, advanced and progressed condition of osteopenia
Symptoms:
- Backache
- Gradual loss of height and an accompanying stooped posture
- Fractures of the spine, wrist or hip
Osteomalacia
Cause – Vitamin D deficiency leading to softening of your bones. Soft bones are more likely to bow and fracture than are harder and healthy bones.
Symptoms:
- Muscle weakness
- Achy bone pain (most common in lower back, pelvis, hips, legs and ribs. Pain may be worse at night or when you are putting weight on the affected bones.
- Decreased muscle tone and leg weakness may cause a waddling gait and make it difficult for you to get around
Hyperparathyroidism
Cause – parathyroid glands in your neck produce too much parathyroid hormone (PTH). This hormone controls calcium, phosphorus, and vitamin D levels in the blood and bone.
When calcium levels are too low, the body responds by making more parathyroid hormone. This hormone causes calcium levels in the blood to rise, as more calcium is taken from the bone and reabsorbed by the intestines and kidney.
In this condition there is abnormally high concentration of parathyroid hormone in the blood resulting in weakening of the bones through loss of calcium
Symptoms:
- Bone pain or tenderness
- Depression and forgetfulness
- Tiredness and weakness
- Fragile bones of the limbs and spine that can break easily
- Increased amount of urine produced and need to urinate more often
- Kidney stones
- Nausea
- Loss of appetite etc
Multiple myeloma
Cause – It is a cancer that forms in a type of white blood cell called a plasma cell. Plasma cells help you fight infections by making antibodies that recognize and attack germs. MM causes cancer cells to accumulate in the bone marrow where they crowd around healthy blood cells.
Symptoms:
- Bone pain, especially in your chest or spine
- Nausea, Constipation, Loss of appetite
- Excessive thirst
- Weakness or numbness in legs, Weight loss
- Frequent infections
- Fatigue, Confusion
Bone metastasis or Skeletal metastases (metastatic bone disease) –
Cause – Cancer metastases that results from primary tumour invasion to the bone
Symptoms:
- Severe pain (dull ache which worsens with time), worse at night
- Bone fractures, Spinal cord compression
- Hypercalcaemia, Anaemia
- Spinal instability, Decreased mobility
Leukaemia
Cause – a malignant progressive disease in which the bone marrow and other blood forming organs produce increased numbers of immature or abnormal leucocytes. These suppress the production of normal blood cells, leading to anaemia and other symptoms
Symptoms:
- New lump or swollen gland in your neck, under your arm or in your groin
- Frequent nose bleeds, bleeding from gums or rectum, or heavy menstruation
- Frequent fevers, Night sweats
- Bone pain
- Loss of appetite, Weight loss
- Tiredness without a known reason etc
Rickets
Cause – Extreme and prolonged vitamin D deficiency leading to softening and weakening of bones in children
Symptoms:
- Delayed growth
- Pain in the spine, pelvis and legs
- Muscle weakness
- Skeletal deformities like bowed legs, thickened wrists and ankles, breastbone projection etc
Scurvy:
Cause – deficiency of vitamin C
Symptoms –
- Malaise, Lethargy
- Pain in gums which interferes with digestion
- Shortness of breath
- Bone pain
- Myalgia (muscle pain)
- Skin changes – roughness, easy bruising, petechiae
- Loosening of teeth
- Dry mouth, Dry eyes etc
Anaemia
Cause: deficiency of red cells or of haemoglobin in the blood
Symptoms –
- Pallor, Fatigue
- Weakness, General malaise
- Poor concentration
- Dyspnoea (shortness of breath), Palpitations etc
Cushing syndrome
Cause – Abnormally high levels of a hormone called cortisol
Symptoms –
- Round-shaped face (moon-face)
- A fatty hump in between your shoulders (buffalo hump)
- Upper body weight gain
- Skin that bruises easily
- Pink or purple stretch marks on your skin
- High blood pressure, Diabetes
- Bone loss, leading to fractures
- Decreased libido and fertility
- Fatigue, Muscle weakness etc
Read related – Osteopenia
Ayurvedic concepts of Osteopenia
As with any disease, we cannot make an exact correlation of osteopenia to any disease condition explained in Ayurveda. But we shall try to draw a hypothesis about the disease and possibilities of treatment.
Since Osteopenia (& osteoporosis) is a condition of bones which lose density and presents no symptoms, we shall try to find its Ayurvedic counter-part which has similar features.
Osteopenia is related to the formation, maintenance and nutritive part of the bone. Thus we will touch the Ayurvedic aspect in that perspective.
Concept of bone formation in Ayurveda:
According to Ayurveda, Asthi Dhatu (Bone tissue) is a Pitruja Avayava (Paternal tissue).
(Embryological concept – All hard tissues or organs in a child are said to be derived from father)
Dhatu Poshana Krama
Dhatu Poshana Krama (Chronology of tissue formation and nutrition):
Dhatu’s or tissues are formed in a chronological order according to Ayurveda. They are formed in an inter-related and inter-locked chain mechanism and also nourish each other (successive tissues).
The formation and nutrition available to each tissue to form its components in a regular and healthy way depends on how best the previous tissue is nourished and enriched from the essence of nutrition provided from the gut (& its precursor dhatu).
In this context: Asthi dhatu is the next dhatu to be formed after Meda dhatu (fat tissue / adipose tissue) and a precursor of Majja Dhatu (bone marrow).
That means to tell that-
- Meda dhatu leads to the formation of Asthi Dhatu and
- Asthi Dhatu leads to the formation of Majja Dhatu.
The precursors of Asthi Dhatu are:
- Meda dhatu – Fat or adipose tissue (immediate precursor)
- Mamsa dhatu – Flesh or muscular tissue (precursor of Meda dhatu)
- Rakta dhatu – Blood tissue (precursor of Mamsa dhatu)
- Rasa dhatu – Lymph or plasma (precursor of Rakta dhatu and a product of Ahara rasa or essence of food supplied from the gut)
The successors of Asthi Dhatu are:
- Majja dhatu – Bone marrow (immediate successor of Meda dhatu)
- Shukra dhatu – Semen or reproductive tissue (successor of Majja dhatu)
- Ojus – Essence of all the above said tissues which represents the strength, immunity and life span of each and every cell
Thus for the Asthi dhatu or bone tissue to be formed in a healthy, qualitative and quantitative way – its precursor dhatu’s should have formed properly.
If there is a pathological increase or depletion of the Asthi dhatu precursors, the bone formation and maintenance takes a beating. The metabolism of bone tissue becomes disturbed leading to loss of density, brittleness, osteopenia which further might progress to osteoporosis.
Similarly if there is a pathological increase or depletion of Asthi dhatu (and its precursors) it will have a disturbing impact on the formation and maintenance of the successive dhatus.
Asthi Dhatu Kshaya:
Asthi Dhatu Kshaya (Depletion of bone tissue) can be a like term which can be used in comparison to Osteopenia. The decrease or depletion of bone tissue can be taken as reduction in bone density. This happens due to:
Agni vikriti
Agni vikriti: (metabolic disturbances)
Almost all the metabolic diseases take place due to the disturbances in Agni (basic core metabolism or metabolic fire in the gut). When the Agni is depleted (Agnimandhya – hypo-functional agni), it leads to Ajeerna (indigestion) and the food is not digested properly. As a result, Ama or intermediate products of digestion is formed which further deteriorates the agni leading to blockage of channels carrying the nutrition. There is inadequate nutrition or nutritive essence (ahara rasa) going to the tissues when this happens. The tissues rare not formed proportionally (quantitatively and qualitatively). This includes Asthi dhatu also.
Among many causes leading to Agnimandhya – a pathological increase of Kapha (watery ingredients of the body) is the chief culprit. It keeps the Agni diluted and hampers its normal functioning.
On the contrary if the Agni is higher (Atyagni – hyper-functional agni) the food is burnt out instead of getting digested. Again there is nothing left for the tissues. This also leads to qualitative and quantitative depletion of the tissues including the Asthi Dhatu (Bone tissue)
Among all the causes leading to Atyagni – a pathological increase of Pitta (Teekshnagni) and Vata (Vishamagni) are the main culprits.
Medo dhatvagni vikriti
Dhatvagni’s are small fractions of the main Jatharagni (belly fire). Dhatvagni’s are present in the Dhatu’s (tissues) and are specific for each tissue. Ex. Rasa dhatu has Rasa dhatvagni, Rakta dhatu has Rakta dhatvagni etc.
These tissue fires take part in tissue metabolism. They convert the gross nutrients (provided by Jatharagni) present in the circulation into minute (micro) nutrients. These minute form of nutrition helps in tissue building and also take part in the formation of the next tissue in the sequence.
Dhatvagni vriddhi and kshaya:
Increase in dhatvagni leads to the depletion of tissue (local) and consequential decrease of the successive dhatu. Decrease in dhatvagni leads to accumulation and blocks in the tissue (local) and subsequent depletion of the successive tissue.
This happens due to the formation of dhatu gata ama (intermediate products of tissue metabolism) which decreases the cellular metabolism grossly and also blocks the channels through which the nutrition to the successive tissues is carried.
In relation to Medo Dhatvagni:
The Medo dhatvagni (fire in fat tissue) digests the nutrition and materials provided to it by its precursor Mamsa dhatu and convert a big part of it into Medo dhatu (local tissue). The remaining portion is used in forming the successive dhatu i.e. Asthi dhatu (bone tissue). Heat, energy, wastes (sweda – sweat in this context) and upadhatu (sub-tissue) are formed in the process.
When Medo dhatvagni decreases, excess meda (fat) are formed (medo vriddhi) i.e. the fat takes all the nutrition and almost sends nothing to the Asthi dhatu. The ama formed in the process blocks the channels which send nutrition to the bones. This leads to fewer nutrients to Asthi dhatu and consequent low density and osteopenia.
When Medo dhatvagni increases there is destruction of fat tissue (medo kshaya) and supply of fewer nutrients to Asthi dhatu. This also leads to osteopenia.
Among the symptoms of Medo dhatu Kshaya is mentioned ‘Svapanam Katyaha’ which means weakness in the hip region (susceptibility to fracture). Hip fractures are common among osteopenia patients.
Asthi Dhatvagni Vikriti
When Asthi dhatvagni decreases, there is excess formation of Asthi dhatu (Asthi vriddhi) and when Asthi dhatvagni increases, there is less formation of Asthi dhatu (Asthi kshaya).
Asthi Kshaya can be compared to osteopenia (& osteoporosis)
Among the symptoms of Asthi Kshaya is mentioned ‘Majjani saushiryam’. If Majja is considered as the matrix or materials which constitute and contribute to the density of the bone, Majja Saushiryam indicates loss of bone density. Asthi Kshaya can be thus compared to Osteopenia and Osteoporosis.
Vata and Asthi
All Dosha’s have their abode in one or the other Dhatu (tissue). Vata is located in Asthi Dhatu. The Vata which has undergone a pathological increase due to Vata disturbing food and lifestyle activities will deplete the Asthi dhatu causing low bone density, osteopenia and osteoporosis. When Vata undergoes pathological decrease, it causes increase in Asthi dhatu.
Thus Vata increase (Vata vriddhi) can be considered one of the causative factors leading to osteopenia. In this sense, all those food and lifestyle activities contributing to Vata vriddhi can be considered as causative factors of Asthi Kshaya vis-à-vis osteopenia (osteoporosis).
Vata Prakopa Karana
Vata Prakopaka Karanani (Causative factors responsible for Vata vitiation):
- Vyayama – Excessive exercises
- Apatarpana – Fasting in excess
- Prapatana – Fall, injury
- Bhanga – Fractures
- Kshaya – Depletion of tissues
- Jaagarat – Excessive vigil (awakening all night)
- Veganam cha vidharanat – Suppression of natural body urges (reflexes)
- Ati shuchi – Excessive administration of cleansing procedures (Panchakarma)
- Shaityadi – Excessive consumption of cold foods and activities
- Traasaat – Fear
- Ruksha – Excessive consumption of dry foods
- Kshobha – Irritation
- Kashaya – Excessive consumption of astringent foods
- Tikta – Excessive consumption of bitter foods
- Katu – Excessive consumption of pungent foods
- Vari-ghanagame – cloudy and rainy season
- Parinate anne – After the digestion of food
- Aparahne – Evening
Among the causative factors for Asthivaha Sroto Dushti (Contamination of channels providing nutrition to bones and help in their formation) Vatala Ahara Vihara (Vata increasing foods and activities) has been explained.
Asthi pradoshaja Roga:
Among the symptoms of Asthi pradoshaja Roga (Diseases due to contamination of bones) – Asthi bheda (splitting pain / fractures in bone?) and Asthi Shula (bone pain) have been mentioned.
Phakka Roga:
Phakka or Fakka Roga has been explained in Ayurvedic Paediatrics and is compared to Rickets.
Acharya Kashyapa tells that ‘A child is said to be suffering from Phakka Roga if he / she does not stand on their foot or walk even after 1 year of age’
Phakka roga is said to be of 3 types:
- Ksheeraja – Drinking breast milk contaminated by morbid Kapha
- Garbhaja – When the mother of the child quickly conceives for one more time she cannot feed the child due to deficit production of breast milk. The child gets debilitated day by day.
- Vyadhija Phakka – Due to the affliction of diseases like fever etc for a prolonged period
Even according to modern medical science, Rickets is taken as a differential diagnosis for osteopenia
Ayurvedic Treatment
Treatment of Osteopenia by Ayurvedic methods should be done on below said lines:
Treating Asthi Dhatu Kshaya on the lines of Asthi pradoshaja vikara (Asthi ashrita roga) –
Panchakarma: Five cleansing measures or evacuation (detoxification) therapies explained in Ayurveda i.e.
- Vamana – Therapeutic emesis (vomiting)
- Virechana – Therapeutic Purgation
- Asthapana Vasti – Decoction enemas
- Anuvasana Vasti – Oil enemas
- Nasya – Nasal instillation of medications
The above said treatments should be adapted according to the condition of the disease and diseased, after considering the disease pathology by all its fragments
Vasti – Among these, Vasti is said to be the best choice. Vasti is the best treatment for vitiated Vayu. We have seen that Vata vitiation is the chief culprit in the causation of osteopenia. Ksheera vasti (Enemas with milk processed with bitter drugs) and Sneha Vasti (enemas with ghee processed using bitter drugs) are very useful in alleviating vitiated Vayu and mitigating osteopenia (and osteoporosis)
Tikta Ksheera – Milk processed with bitter drugs shall be used to drink and also for enemas
Tikta Ghrita – Ghee processed with decoction of bitter drugs shall be used for drinking purpose and also for enemas
Treating Vayu:
- Sneha – Administration of medicated oils / ghee, Massage, oil pouring etc
- Sweda – Steaming / sudation / sweating therapy
- Mridu shodanam – Evacuation treatment (mild cleansing treatments like Virechana etc)
- Svadu bhojana – Consuming sweet foods
- Amla bhojana – consuming sour foods
- Lavana bhojana – consuming salt foods
- Ushna bhojana – Hot and fresh foods
- Abhyangam – Massage with herbal oils
- Mardana – Tapping the body with closed fists after application of vata alleviating oils
- Seka – Pouring of medicated oils over the body in streams
- Paishtika Madhya – Alcohol or fermented products prepared with flours
- Goudika Madhya – Alcohol or fermented products prepared with jaggery
- Snigdhoshna Vasti – Medicated enemas with oils and ghee, given luke warm
- Deepana pachana sneha – Oils and ghee processed with deepana (appetizer) and pachana (digestant) drugs
Avoiding Vata prakopaka ahara vihara
Avoiding food and life style activities which aggravate Vata (explained above)
Correction of Agni, Ajeerna and Ama:
- Disturbance of metabolism, indigestion and metabolites are said to be the initial culprits (culprits at the foundation) of osteopenia.
- Loss of appetite, indigestion and any symptom related to upper or lower gastro-intestinal tract persisting for a longer duration should not be taken lightly.
- They should be corrected by administration ghee processed with deepana (fire stimulating or appetizing) drugs and pachana (digestion promoting or ama destroying) drugs or the same drugs mixed in ghee. Medicines can be given in other forms also – Churna, Kashayam, etc
Ex: Ardhraka Ghrita, Guggulutiktakam Ghritam / Kashayam, Tiktaka Ghritam / Kashayam, Pippalyadi Ghritam, Indukantam Ghritam, Trikatu Churna, Panchakola churna etc.
- The same medications correct errors of dhatugata agnimandhya (low tissue metabolism) and strengthen the tissues, the medo dhatvagni and asthi dhatvagni in this case.
Medoroga Chikitsa
Medo-chikitsa / Medoroga chikitsa:
- Since Meda or fat is the immediate precursor of Asthi dhatu, treatment and medications to prevent or reduce accumulation of fat in the body should be administered, especially if the patient has a weight putting tendency or is obese and having family history of osteoporosis or osteopenia.
- Virechana (Therapeutic purgation), Lekhana Vasti (fat eliminating enemas) and Udwarthana (massage done with herbal powders in the reverse direction of hair follicles) would provide benefit in these cases.
- Anti-obesity medications should be given to reduce weight and fat. Ex: Medohara vidangadi lauha, Navaka Guggulu, Varadi Kashayam, Varanadi Kashayam, Guggulutiktakam Kashayam
Asthigata, Sandhigata Vata Chikitsa
Asthigata Vata and Sandhigata Vata chikitsa –
- The above said 2 conditions are explained in Vata Vyadhi Though they are painful conditions caused by vitiated vayu (pain doesn’t exist in osteopenia), the treatment and medicines adapted in these 2 conditions can also be adapted in case of osteopenia because all those remedies take care of vitiated Vata and damage occurring in the bones.
- The treatments and medications of both these conditions are done on the lines of Vata Vyadhi treatment (explained above in context of ‘Treat Vayu’)
Treating on lines of Bhagna Chikitsa (fracture treatment):
In any case of fracture, the bone should be reset before trying any medicine.
General treatment:
- Seka – Stream pouring of medicated oils, milk etc
- Lepa – Application of medicinal pastes
- Bandhana – Bandages
- Sheta upachara – Cold treatments (remedies)
Ayurvedic medicines, herbs
Medications:
Asthishrunkala (Cissus quadrangularis) is the best option in fractures and dislocations
- Medicated ghee prepare with this drug is taken orally
- The juice of the plant can be given with ghee
- Macerated stem of the fresh plant is used for application over fracture
Babul tree – Bark or seed powder of Babul is given with honey for fracture healing
Lashunadi Kalka – Paste of equal parts of Garlic, Lac, honey and sugar is given mixed in ghee
Pravala Bhasma – Pravala Bhasma (ash of coral) is given with honey or ghee
Arjuna twak churna – Powder of bark of Terminalia arjuna is given with milk
Shatadhauta Ghrita: Ghee processed (washed) with medicinal herbs (their decoctions) for 100 times is mixed with Shali pishti (rice flour) and applied over the fractures
Laksha-godhumadi yoga: Powder of lac, wheat flour and powder of Arjuna bark (Terminalia arjuna) mixed with ghee
Rasonadi yoga: Paste of Garlic, honey, Lac, ghee and sugar
Guggulu (Commiphora mukul) preparations
- Lakshadi Guggulu
- Aabhadi Guggulu
Treating on the lines of Phakka Roga:
Ghrita pana: (medicated ghee for drinking)
- Kalyanaka Ghritam
- Shatpala Ghritam
- Amruta Ghritam
Shodhana (cleansing medicines):
After the child is saturated by Snehana (drinking medicated ghee as said above) Shodhana, especially Virechana (purgation) should be given after 7 days by administering Trivrit Ksheera – milk processed with Trivrit (Operculina turpethum)
Brahmi Ghrita: After the evacuation process (Shodhana), Brahmi Ghrita should be given
Diet: Mamsayusha (meat soup), Shali (cooked rice), Siddha ksheera (medicated milk etc
Vasti – Medicated enemas
Svedana – Steaming or fomentation with herbal decoctions or milk
Udvartana- Powder massage done in a reverse direction (upward)
Best formulations for osteopenia:
- Maharasnadi Kashayam
- Dhanwantaram Kashayam
- Ashwagandharishtam
- Dashamoolarishtam
- Balarishtam
- Aabhadi Guggulu
- Lakshadi Guggulu
- Trayodashanga Guggulu
- Yogaraja Guggulu
- Medohara Vidangadi Lauha
- Navaka Guggulu
- Vatagajankusha Rasa
- Vata vidhwamsini Rasa
- Tiktaka Ghritam
- Guggulutiktaka Ghritam
- Shatavari Ghritam
- Ashwagandhadi Ghritam
- Mukta shukti Bhasma / Mukta shukti pishti – Pearl calcium
- Jawar Mohar Pishti
- Kamadudha Rasa
- Mukta Bhasma / Mukta pishti
- Shringa Bhasma
- Akik pishti
- Gandha Tailam
- Ksheerabala tailam 101
- Dhanwantaram 101
Important drugs used for treating osteopenia:
- Asthishrunkala – Cissus quadrangularis
- Amalaki – Emblica officinalis
- Arjuna – Terminalia arjuna
- Equisetum arvense – Horsetail
- Laksha – Lac
- Guggulu – Commiphora mukul
- Triphala – Fruits of Terminalia chebula, Terminalia bellirica and Emblica officinalis
- Pravala – Coral
- Tila – Sesame seeds
- Babul – Vachellia nilotica / Acacia nilotica
- Symphytum officinale – Comfrey roots
- Angelica archangelica – Wild celery / Holy Ghost
- Shigru – Moringa oleifera (drumstick)
- Ashoka – Saraca indica
- Ashwagandha – Withania somnifera
- Nagabala – Grewia hirsute
- Shatavari – Asparagus racemosus
Commonly used drugs for treating osteopenia:
- Bisphosphonates (alendronate, risedronate and bandronate)
- Selective oestrogen receptor modulators (SERM’s) such as raloxifene, oestrogen, calcitonin and teriparatide
- Strontium ranelate has shown to build bone both by slowing the work of osteoclasts and stimulating osteoblasts
- Raloxifene
- Hormone replacement
Studies
- Actual benefits of the drugs in treatment of osteopenia may be marginal. Approximately 270 women with osteopenia might need to be treated with drugs for 3 years so that one of them could avoid a single vertebral fracture
- Strontium ranelate approved by 27 European countries has shown to build bone both by slowing the work of osteoclasts and stimulating osteoblasts
- The European Pharmaco-vigilance Risk Assessment Committee recommended that Strontium ranelate should be cautiously used in treatment of osteoporosis. Studies have shown an increased non-fatal myocardial infarction in patients with ischaemic heart disease or uncontrolled hypertension patients.
- Strontium is also available as Strontium lactate, Strontium gluconate, Strontium carbonate and Strontium citrate. Food sources include spices (especially basil), seafood, whole grains, root and leafy vegetables and legumes. Strontium should not be used with calcium supplements to improve absorption.
Conclusion
Osteopenia may be a symptom-less disease or condition but remember that it is slowly eclipsing your bone health!!
Take care of your bones before they end up with serious issues…
Prevention is the best option in the management of Osteopenia…
You have the best remedies for preventing and treating Osteopenia in Ayurveda. But don’t forget to consult an Expert Ayurveda Doctor for an opinion before starting on with anything because self-medication might be harmful.





13 comments
SHIVA SHANKER GUPTA
VERY INFORMATIVE. Thanks. Write about OLD AGE diseases.
Dr J V Hebbar MD(Ayu)Author
Thanks. Will be covering about old age disorders shortly.
Galochka
Very nice article. I have a question about caned sardines. Although they have a lot of calcium, caned food is not good to eat per Ayurveda. Or is it o’key in this case? Thanks.
Dr J V Hebbar MD(Ayu)Author
Hi, Canned foods are not good as per Ayurveda.
arja P
which of the above formulation is best for calcium deficiency or low bone density and for increasing hemoglobin level?
Dr Malini Bhat
Sir do consult a ayurvedic physician seeing the bone density tests he/she might prescribe you the medicines.
Note: Duration of internal medications are better to be decided after analysing the condition and prognosis of your body and problem. for this it is better to consult an Ayurveda doctor directly.
Dr. HITESH Acharya
Pt. Having diabetes with ostopenia Amrtarishtam or ashwagandharistam which will be best?
Dr J V Hebbar MD(Ayu)Author
Because the patient is diabetic, both are not recommended
KK
Hello Dr. JV
Doctor has told that my daughter ( 9 years ) has bone demineralization. Is that same as ( or related ) to Osteopenia ? Please explain. If Ayurveda has good solutions for demineralization, would like to consult you.
Thanks for writing articles on various topics. It is very helpful.
Dheeraj
Is there any scientific research data on Babula seed powder with honey heals bone fracture?
Dr J V Hebbar MD(Ayu)Author
I did not find.
OVRajamohan Rajamohan
very informative article. Please let us have similar article on enlarged prostate gland in men.
Dr J V Hebbar MD(Ayu)Author
Please read here
https://www.easyayurveda.com/2021/07/09/benign-prostatic-hyperplasia/